Metabolic Syndrome
Explore the connection between gut microbiome imbalances and metabolic syndrome, and discover evidence-based approaches for managing metabolic health through microbiome optimization.
Common Symptoms
Microbiome Imbalances
Research has identified the following microbiome patterns commonly associated with this condition:
- Reduced microbial diversity
- Increased Firmicutes to Bacteroidetes ratio
- Decreased butyrate-producing bacteria
- Increased opportunistic pathogens
Understanding Metabolic Syndrome and the Microbiome Connection
Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. These conditions include increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels.
A diagnosis of metabolic syndrome is typically made when an individual has at least three of the following five factors:
- Abdominal obesity (waist circumference > 40 inches in men or > 35 inches in women)
- Triglyceride level ≥ 150 mg/dL
- HDL cholesterol < 40 mg/dL in men or < 50 mg/dL in women
- Blood pressure ≥ 130/85 mmHg
- Fasting glucose ≥ 100 mg/dL
In recent years, compelling evidence has emerged linking gut microbiome composition to metabolic health. Individuals with metabolic syndrome typically show distinct alterations in their gut microbiota compared to metabolically healthy individuals.
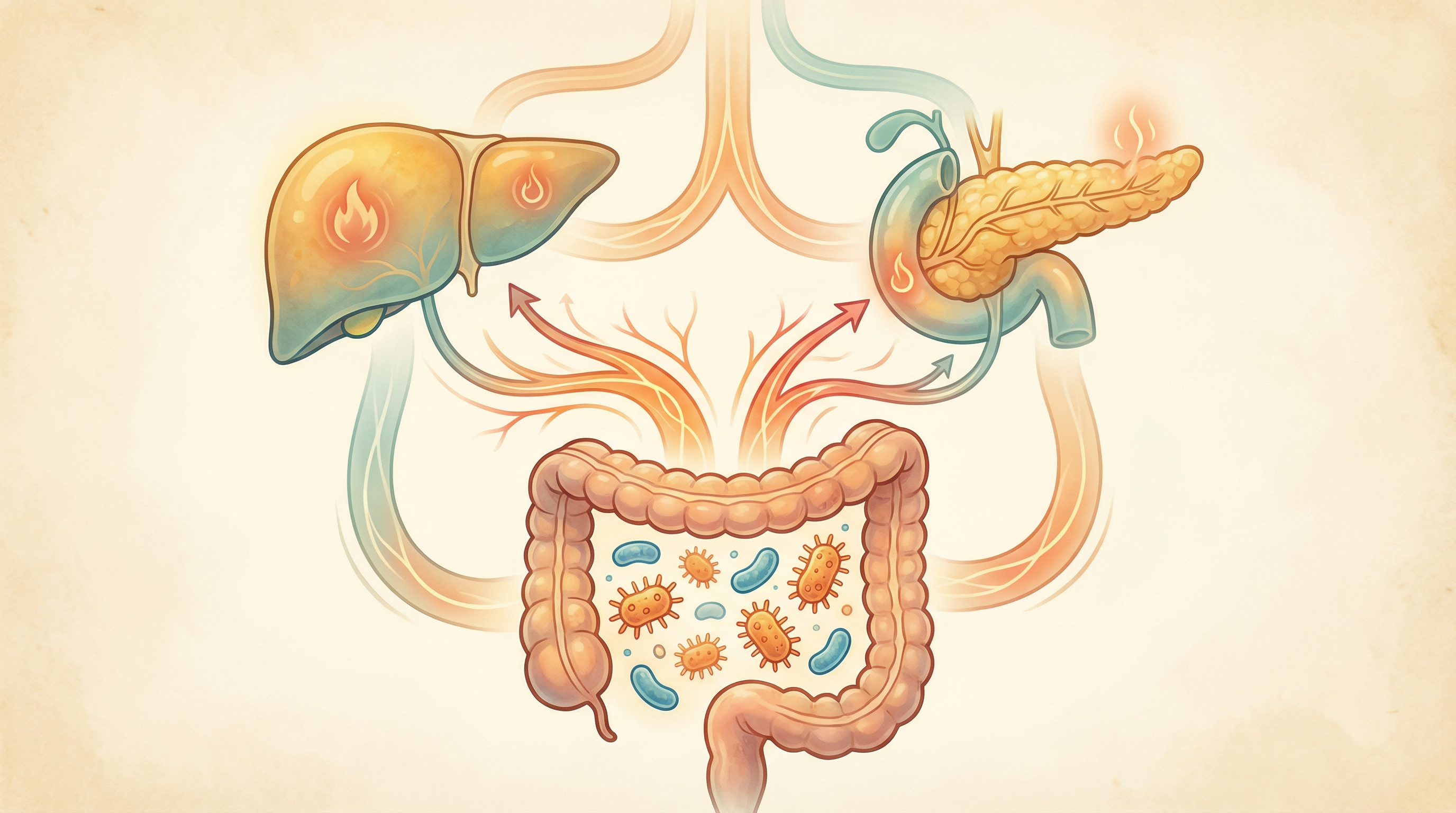
How Gut Dysbiosis Influences Metabolic Syndrome Development
Several mechanisms connect gut microbiome imbalances to metabolic syndrome. The gut microbiota plays a pivotal role in metabolic syndrome pathogenesis through dysbiosis-induced chronic inflammation and insulin resistance.[1] Faecal carbohydrates, particularly host-accessible monosaccharides, are increased in individuals with insulin resistance and are associated with microbial carbohydrate metabolism and host inflammatory cytokines.[2]
Intestinal Barrier Function
Dysbiosis can compromise the intestinal barrier, leading to increased intestinal permeability ("leaky gut"). This allows bacterial components like lipopolysaccharide (LPS) to enter the bloodstream, triggering systemic inflammation and insulin resistance. A strong correlation and partial causal association exists between gut microbiota composition and insulin resistance.[3]
Short-Chain Fatty Acid Production
Beneficial gut bacteria ferment dietary fiber to produce short-chain fatty acids (SCFAs), particularly butyrate, which:
- Improve insulin sensitivity
- Reduce inflammation
- Regulate appetite and energy expenditure
- Support intestinal barrier integrity
Individuals with metabolic syndrome typically show reduced SCFA production.
Bile Acid Metabolism
Gut microbes transform primary bile acids into secondary bile acids, which act as signaling molecules that regulate glucose and lipid metabolism. Dysbiosis can disrupt this process, contributing to metabolic dysfunction.
Choline and TMAO
Certain gut bacteria convert dietary choline to trimethylamine (TMA), which is further metabolized to trimethylamine N-oxide (TMAO). Elevated TMAO levels are associated with increased cardiovascular risk, a key component of metabolic syndrome. Research shows elevated TMAO levels represent a key link between gut microbiota-derived metabolites and metabolic syndrome pathogenesis.[4]
Key Microorganisms in Metabolic Syndrome
Several specific microorganisms have been implicated in metabolic health:
Akkermansia muciniphila
This mucin-degrading bacterium has emerged as a promising probiotic candidate for metabolic syndrome. Studies show that:
- A. muciniphila levels are typically reduced in individuals with obesity and metabolic syndrome
- Supplementation with A. muciniphila improves insulin sensitivity and reduces inflammatory markers in animal models and human trials
- It strengthens the intestinal barrier and modulates immune responses
Faecalibacterium prausnitzii
This beneficial bacterium:
- Is a major butyrate producer
- Has anti-inflammatory properties
- Is typically reduced in individuals with metabolic syndrome
- Correlates positively with insulin sensitivity
Bifidobacterium species
These beneficial bacteria:
- Produce acetate and lactate, which can be converted to butyrate
- Strengthen the intestinal barrier
- Reduce inflammation
- Are often depleted in metabolic syndrome
Prevotella copri
This bacterium shows complex relationships with metabolic health:
- Some strains improve glucose metabolism and insulin sensitivity
- Other strains may promote inflammation in certain contexts
- Its effects appear to be influenced by diet and genetic factors

Microbiome-Based Approaches for Metabolic Syndrome Management
Emerging research supports several microbiome-focused strategies for managing metabolic syndrome:
Dietary Modifications
Specific dietary patterns can beneficially modulate the gut microbiome and improve metabolic health:
Mediterranean Diet
Rich in fruits, vegetables, whole grains, olive oil, and fish, this diet:
- Increases microbial diversity
- Enhances SCFA production
- Reduces inflammation
- Improves metabolic parameters
Evidence Level: Strong
High-Fiber Diet
Dietary fibers serve as prebiotics that nourish beneficial bacteria:
- Soluble fibers improve glycemic control and lipid profiles
- Insoluble fibers support gut barrier function and microbial diversity
- Resistant starch enhances butyrate production
Evidence Level: Strong
Intermittent Fasting
Periodic fasting regimens can:
- Promote beneficial shifts in gut microbiota composition
- Enhance metabolic flexibility
- Reduce inflammation
- Improve insulin sensitivity
Evidence Level: Moderate
Probiotics
Specific probiotic strains show promise for metabolic syndrome management:
- Akkermansia muciniphila: Improves insulin sensitivity and reduces inflammatory markers
- Lactobacillus plantarum: Reduces body fat and improves lipid profiles
- Bifidobacterium lactis: Enhances glucose metabolism and reduces inflammation
- Multi-strain formulations: Often show better results than single strains
Evidence Level: Moderate
Prebiotics
Non-digestible food components that selectively feed beneficial bacteria:
- Inulin: Enhances Bifidobacteria and improves metabolic parameters
- Fructooligosaccharides (FOS): Improve lipid profiles and insulin sensitivity
- Galactooligosaccharides (GOS): Reduce inflammatory markers and enhance beneficial bacteria
Evidence Level: Moderate to Strong
Synbiotics
Combinations of probiotics and prebiotics that work synergistically:
- May provide more comprehensive benefits than either component alone
- Show promise for improving multiple metabolic parameters simultaneously
Evidence Level: Preliminary to Moderate

Clinical Evidence and Research Highlights
Recent studies have provided compelling evidence for the microbiome-metabolic syndrome connection:
A 2023 study in Nature demonstrated that gut microbial carbohydrate metabolism directly contributes to insulin resistance, with faecal monosaccharides elevated in insulin-resistant individuals.[2]
A 2024 systematic review and meta-analysis found that gut microbiota-targeted interventions significantly reduced fasting glucose, HbA1c, HOMA-IR, total cholesterol, LDL-C, and triglycerides, offering a potential therapeutic strategy for managing metabolic diseases.[5]
Research has established that modulation of the gut microbiome via supplementation therapies such as probiotics, prebiotics, synbiotics, and postbiotics positively influences metabolic health by improving glucose metabolism and lipid profiles.
A 2025 comprehensive review confirmed that targeted interventions like probiotics offer promising therapeutic approaches for metabolic syndrome through addressing dysbiosis-induced chronic inflammation.[1]
The Role of Personalized Nutrition and Microbiome Analysis
Given the complex interplay between individual microbiome compositions, genetics, diet, and lifestyle factors, personalized approaches to metabolic syndrome management are likely to be most effective:
- Microbiome testing: Analyzing gut microbiome composition to identify specific imbalances
- Metabolic phenotyping: Assessing individual responses to different foods and nutrients
- Targeted interventions: Selecting specific dietary patterns, probiotics, and prebiotics based on individual profiles
- Continuous monitoring: Tracking changes in microbiome composition and metabolic parameters over time
Future Directions in Microbiome-Based Metabolic Health Optimization
The field of microbiome research in metabolic syndrome is rapidly evolving, with several promising developments on the horizon:
- Next-generation probiotics: Novel beneficial strains like Akkermansia muciniphila and Faecalibacterium prausnitzii
- Precision prebiotics: Compounds designed to selectively nourish specific beneficial bacteria
- Postbiotics: Beneficial bacterial metabolites and components that may provide benefits without requiring live organisms
- Microbiome editing: Targeted approaches to modify gut microbiome composition
- Microbiome-informed drug development: Medications that work by modulating the microbiome or whose efficacy is enhanced by specific microbial profiles
Key Takeaways
- Metabolic syndrome is strongly associated with alterations in gut microbiome composition and function
- Specific beneficial bacteria, particularly Akkermansia muciniphila and butyrate-producing species, play key roles in metabolic health
- Dietary patterns that support gut microbiome health, especially the Mediterranean diet and high-fiber approaches, can improve metabolic parameters
- Probiotics, prebiotics, and their combinations show promise for metabolic syndrome management
- Personalized approaches targeting individual microbiome compositions are likely to be most effective
- Emerging research is paving the way for more targeted, microbiome-focused treatments for metabolic syndrome
Research Summary
Emerging research has established strong connections between gut microbiome composition and metabolic health, with studies showing that microbiome transplantation from lean donors can improve insulin sensitivity in individuals with metabolic syndrome. Specific bacterial species, particularly Akkermansia muciniphila, have shown promise in improving metabolic parameters in clinical trials.
References
- Singh A, Verma A, Ashraf S, et al.. Role of gut microbiota in the pathogenesis of metabolic syndrome: an updated comprehensive review from mechanisms to clinical implications. Annals of Medicine and Surgery. 2025;87(9):5851-5861. doi:10.1097/MS9.0000000000003656 ↩
- Takeuchi T, Kubota T, Nakanishi Y, et al.. Gut microbial carbohydrate metabolism contributes to insulin resistance. Nature. 2023;621:389-395. doi:10.1038/s41586-023-06466-x ↩
- Ji H, Su S, Chen M, et al.. The role of gut microbiota in insulin resistance: recent progress. Frontiers in Microbiology. 2025;16:1633029. doi:10.3389/fmicb.2025.1633029 ↩
- Naghipour S, Cox AJ, Peart JN, et al.. Circulating levels of TMAO and its precursors across healthy and early cardiometabolic disease phenotypes. Diabetology & Metabolic Syndrome. 2024;16(1):132. doi:10.1186/s13098-024-01368-y ↩
- Mederle AL, Dima M, Stoicescu ER, et al.. Impact of Gut Microbiome Interventions on Glucose and Lipid Metabolism in Metabolic Diseases: A Systematic Review and Meta-Analysis. Life. 2024;14(11):1485. doi:10.3390/life14111485 ↩
