Anxiety and Depression
Explore the emerging science behind the gut-brain axis and how your microbiome influences anxiety, depression, and overall mental wellbeing.
Common Symptoms
Microbiome Imbalances
Research has identified the following microbiome patterns commonly associated with this condition:
- Reduced microbial diversity
- Lower Lactobacillus and Bifidobacterium levels
- Increased inflammatory bacteria
Understanding Anxiety and Depression
Anxiety and depression are among the most common mental health conditions worldwide, affecting hundreds of millions of people and representing a leading cause of disability. While traditionally viewed as primarily brain-based disorders, a paradigm shift is occurring as research increasingly reveals the crucial role of the gut microbiome in mental health.[1]
Anxiety disorders encompass a spectrum of conditions characterized by excessive worry, fear, and related behavioral disturbances. Depression (major depressive disorder) involves persistent feelings of sadness, emptiness, and loss of interest or pleasure, along with physical symptoms like sleep disturbances, fatigue, and appetite changes. Both conditions significantly impact quality of life and can be challenging to treat effectively with conventional approaches alone.
The complex relationship between these mental health conditions and the microbiome offers new insights into their development and potential treatment approaches that extend beyond traditional psychiatric interventions.
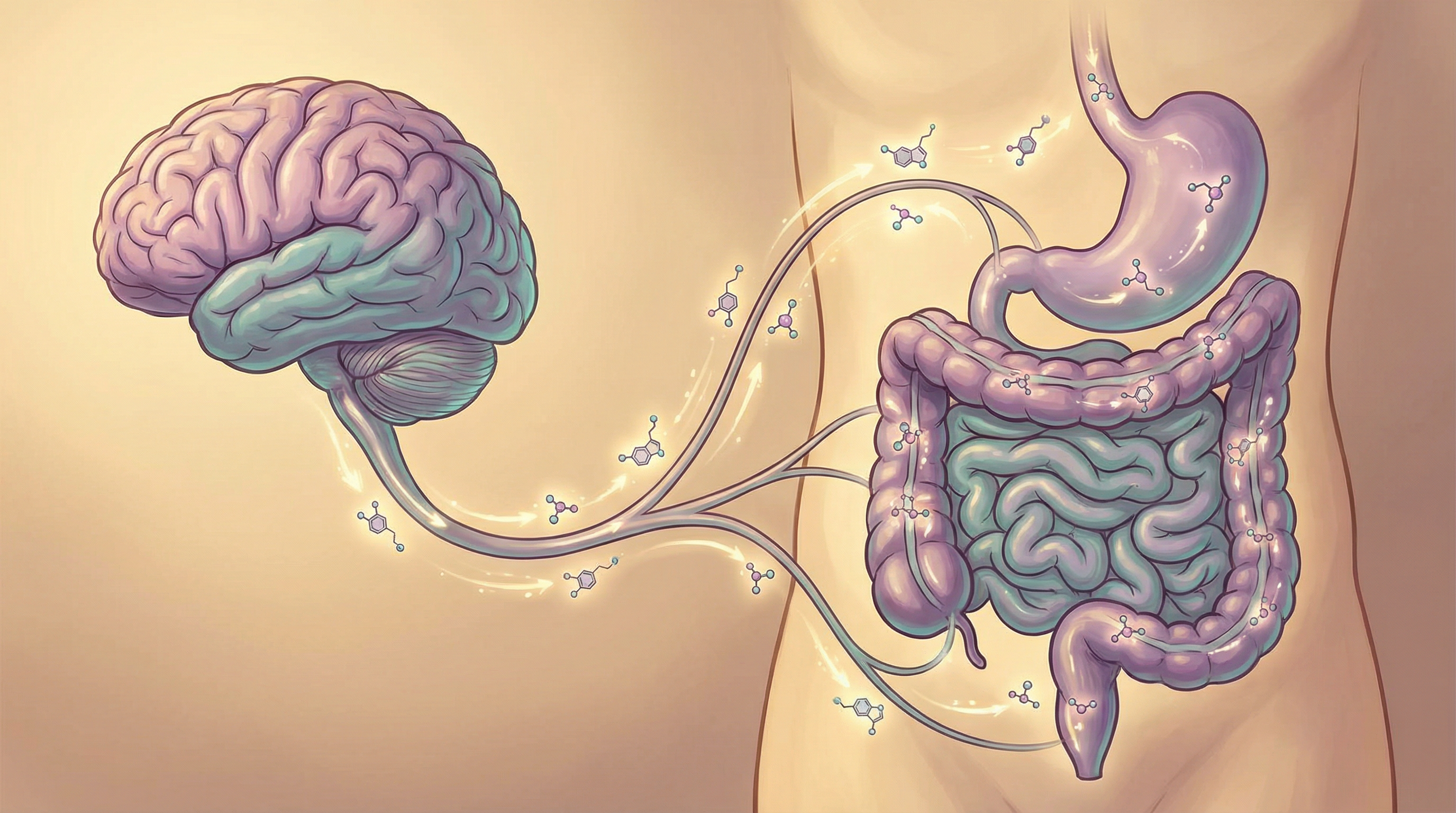
The Gut-Brain Axis: A Two-Way Communication System
The gut-brain axis represents a bidirectional communication network connecting the central nervous system with the enteric nervous system and the gut microbiome.[1] This complex system operates through multiple pathways:
Vagus Nerve Signaling
The vagus nerve serves as a direct communication highway between gut and brain, transmitting signals in both directions. Gut bacteria can stimulate vagal afferents, influencing brain function and behavior.
Neurotransmitter Production
Gut bacteria produce or influence the production of neurotransmitters including serotonin, GABA, dopamine, and norepinephrine—key chemical messengers involved in mood regulation.
Immune System Modulation
The microbiome shapes immune responses that can affect neuroinflammation, which is increasingly recognized as a contributor to depression and anxiety.[2]
Microbial Metabolites
Bacterial metabolites like short-chain fatty acids (SCFAs) influence brain function through multiple mechanisms, including epigenetic regulation of gene expression in the brain.
A landmark 2019 study published in Nature Microbiology identified specific gut bacteria associated with quality of life and depression.[3] The researchers found that Faecalibacterium and Coprococcus were consistently associated with higher quality of life indicators, while Dialister and Coprococcus were depleted in individuals with depression, even after controlling for antidepressant use.
Key Microorganisms in Mental Health
Several specific microorganisms have been implicated in mental health, with their presence or absence potentially influencing anxiety and depression:
Lactobacillus rhamnosus
Impact: Beneficial, often reduced in anxiety and depression Function: Modulates GABA receptors in the brain, reduces stress-induced corticosterone, and influences emotional behavior. A landmark study demonstrated that psychobiotic Lactobacillus strains reduce anxiety-like behavior through vagal signaling and modulation of central GABA receptors.[4]
Bifidobacterium longum
Impact: Beneficial, typically depleted in depression Function: Reduces anxiety-like behaviors, influences stress responses, and may improve cognitive function
Faecalibacterium prausnitzii
Impact: Beneficial, often reduced in depression Function: Major butyrate producer with anti-inflammatory properties; associated with higher quality of life scores[3]
Bacteroides fragilis
Impact: Mixed; can have beneficial effects on neuroinflammation Function: Produces polysaccharide A (PSA) that can modulate neuroinflammation and potentially influence anxiety-like behaviors
The relationship between these microorganisms and mental health is complex and bidirectional.[2] Stress and psychological factors can alter gut microbiome composition, while changes in the microbiome can influence stress responses and emotional behavior. This creates potential feedback loops that may contribute to the chronicity of anxiety and depression.
Importantly, research suggests that the overall microbial community structure and diversity may be more relevant than individual species, highlighting the importance of a balanced, diverse microbiome for optimal mental health.
Microbiome-Based Approaches for Mental Health
Emerging research supports several microbiome-focused strategies for supporting mental health:[5]
Psychobiotics
Specific probiotic strains with documented mental health benefits, particularly Lactobacillus rhamnosus, Bifidobacterium longum, and Lactobacillus acidophilus. Clinical trials show these may reduce symptoms of anxiety and depression in some individuals. A systematic review demonstrated associations between altered gut microbiota composition and both anxiety and depression symptoms.[6] A meta-analysis showed transdiagnostic patterns of gut microbiota alterations across psychiatric disorders including depression and anxiety.[7] Evidence Level: Moderate
Mediterranean Diet
Rich in polyphenols, omega-3 fatty acids, and fiber, this dietary pattern promotes beneficial gut bacteria and has been associated with lower rates of depression.[8] The SMILES trial demonstrated that dietary improvement can be an effective treatment strategy for major depression. Evidence Level: Strong
Prebiotics
Dietary fibers that selectively feed beneficial bacteria can improve gut microbiome composition and potentially influence mood. Galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) have shown particular promise for reducing stress responses. Evidence Level: Preliminary to Moderate
Fermented Foods
Foods like yogurt, kefir, sauerkraut, and kimchi contain live beneficial bacteria and have been associated with reduced anxiety and depression symptoms in observational studies and small clinical trials. Evidence Level: Preliminary
These microbiome-based approaches are most effective when integrated with conventional mental health treatments, including psychotherapy, medication when appropriate, stress management, physical activity, and good sleep hygiene. The optimal approach likely involves addressing both psychological and microbiome factors simultaneously.

The Microbiome-Inflammation-Depression Connection
A growing body of evidence supports the "inflammatory hypothesis of depression," which proposes that inflammation plays a causal role in at least some forms of depression. The microbiome is a key regulator of inflammatory processes:
Key Aspects of the Microbiome-Inflammation-Depression Connection
- Intestinal Permeability: Dysbiosis can increase gut permeability, allowing bacterial components like lipopolysaccharide (LPS) to trigger systemic inflammation
- Cytokine Production: The microbiome influences the production of pro-inflammatory cytokines like IL-6, IL-1β, and TNF-α, which can affect brain function and behavior
- Tryptophan Metabolism: Inflammation activates the enzyme IDO, shifting tryptophan metabolism away from serotonin production and toward the kynurenine pathway, potentially contributing to depression
- Microglial Activation: Systemic inflammation can activate microglia (brain immune cells), leading to neuroinflammation associated with depression
This connection explains why conditions involving chronic inflammation, such as autoimmune disorders and inflammatory bowel disease, are associated with higher rates of depression. It also suggests that approaches targeting the microbiome could potentially address a root cause of depression in some individuals, particularly those with elevated inflammatory markers.
Clinical Evidence and Research Highlights
Recent studies have provided important insights into the gut-brain connection:
A 2016 study demonstrated that transferring gut microbiota from depressed patients to rats induced depressive-like behaviors, providing direct evidence for a causal role of the microbiome in depression.[9]
The SMILES trial (2017) showed that a Mediterranean-style dietary intervention significantly improved depression symptoms compared to a social support control group, with effects maintained at 3-month follow-up.[8]
A 2019 meta-analysis of controlled clinical trials found that both probiotics and prebiotics had significant effects in reducing symptoms of depression and anxiety.[5]
Future Directions in Microbiome-Mental Health Research
The field of microbiome-mental health research is rapidly evolving, with several promising directions:
Personalized Approaches
Research is increasingly focusing on identifying specific microbiome signatures that might predict response to different treatments, potentially enabling more personalized approaches to mental health care.
Novel Interventions
Beyond traditional probiotics, researchers are exploring next-generation approaches including:
- Psychobiotics: Specifically engineered probiotics designed to produce neuroactive compounds
- Postbiotics: Beneficial metabolites produced by microorganisms that may have direct effects on mental health
- Fecal Microbiota Transplantation (FMT): While still experimental for mental health conditions, early research shows potential for treatment-resistant depression
Microbiome Testing
Advances in microbiome testing technology are making it increasingly feasible to assess individual microbiome compositions and potentially identify imbalances relevant to mental health.
The integration of microbiome science into mental health care represents a paradigm shift toward a more holistic understanding of these complex conditions.[1] While much research remains to be done, the evidence to date suggests that nurturing a healthy gut microbiome may be an important component of comprehensive mental health care.
Research Summary
Emerging research on the gut-brain axis suggests that microbiome composition can influence mental health through various pathways including neurotransmitter production, inflammation regulation, and vagus nerve signaling. Clinical studies have shown that certain probiotic strains may help reduce symptoms of anxiety and depression.
References
- Cryan JF, O'Riordan KJ, Cowan CSM, et al.. The microbiota-gut-brain axis. Physiological Reviews. 2019;99(4):1877-2013. doi:10.1152/physrev.00018.2018 ↩
- Foster JA, Rinaman L, Cryan JF.. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiology of Stress. 2017;7:124-136. doi:10.1016/j.ynstr.2017.03.001 ↩
- Valles-Colomer M, Falony G, Darzi Y, et al.. The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology. 2019;4(7):623-632. doi:10.1038/s41564-019-0431-8 ↩
- Bravo JA, Forsythe P, Chew MV, et al.. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences. 2011;108(39):16050-16055. doi:10.1073/pnas.1102999108 ↩
- Liu RT, Walsh RFL, Sheehan AE.. Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials. Neuroscience & Biobehavioral Reviews. 2019;102:13-23. doi:10.1016/j.neubiorev.2019.03.023 ↩
- Simpson CA, Mu A, Haslam N, et al.. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. Journal of Affective Disorders. 2020;266:429-446. doi:10.1016/j.jad.2020.01.124 ↩
- Nikolova VL, Cleare AJ, Stone JM, Young AH.. Perturbations in gut microbiota composition in psychiatric disorders: a review and meta-analysis. JAMA Psychiatry. 2021;78(12):1343-1354. doi:10.1001/jamapsychiatry.2021.2573 ↩
- Jacka FN, O'Neil A, Opie R, et al.. A randomised controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial). BMC Medicine. 2017;15(1):23. doi:10.1186/s12916-017-0791-y ↩
- Kelly JR, Borre Y, O'Brien C, et al.. Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. Journal of Psychiatric Research. 2016;82:109-118. doi:10.1016/j.jpsychires.2016.07.019 ↩
