Atopic Dermatitis (Eczema)
Discover the crucial connection between your microbiome and atopic dermatitis (eczema), and learn evidence-based approaches for managing symptoms through skin and gut health.
Common Symptoms
Microbiome Imbalances
Research has identified the following microbiome patterns commonly associated with this condition:
- Staphylococcus aureus overgrowth
- Reduced skin microbiome diversity
- Decreased Bifidobacteria in gut
- Increased intestinal permeability
Understanding Atopic Dermatitis
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition characterized by red, itchy, and inflamed skin. It typically begins in childhood and may persist or recur throughout life, significantly impacting quality of life through intense itching, sleep disturbance, and visible skin changes.
Eczema is part of the "atopic march," a progression of allergic conditions that often begins with eczema in infancy and may later include food allergies, allergic rhinitis (hay fever), and asthma. This connection highlights the systemic nature of the condition and its relationship to immune dysregulation.
While traditionally viewed as primarily a skin barrier dysfunction and immune disorder, mounting evidence reveals that both the skin and gut microbiomes play crucial roles in eczema development, progression, and symptom severity.[1]
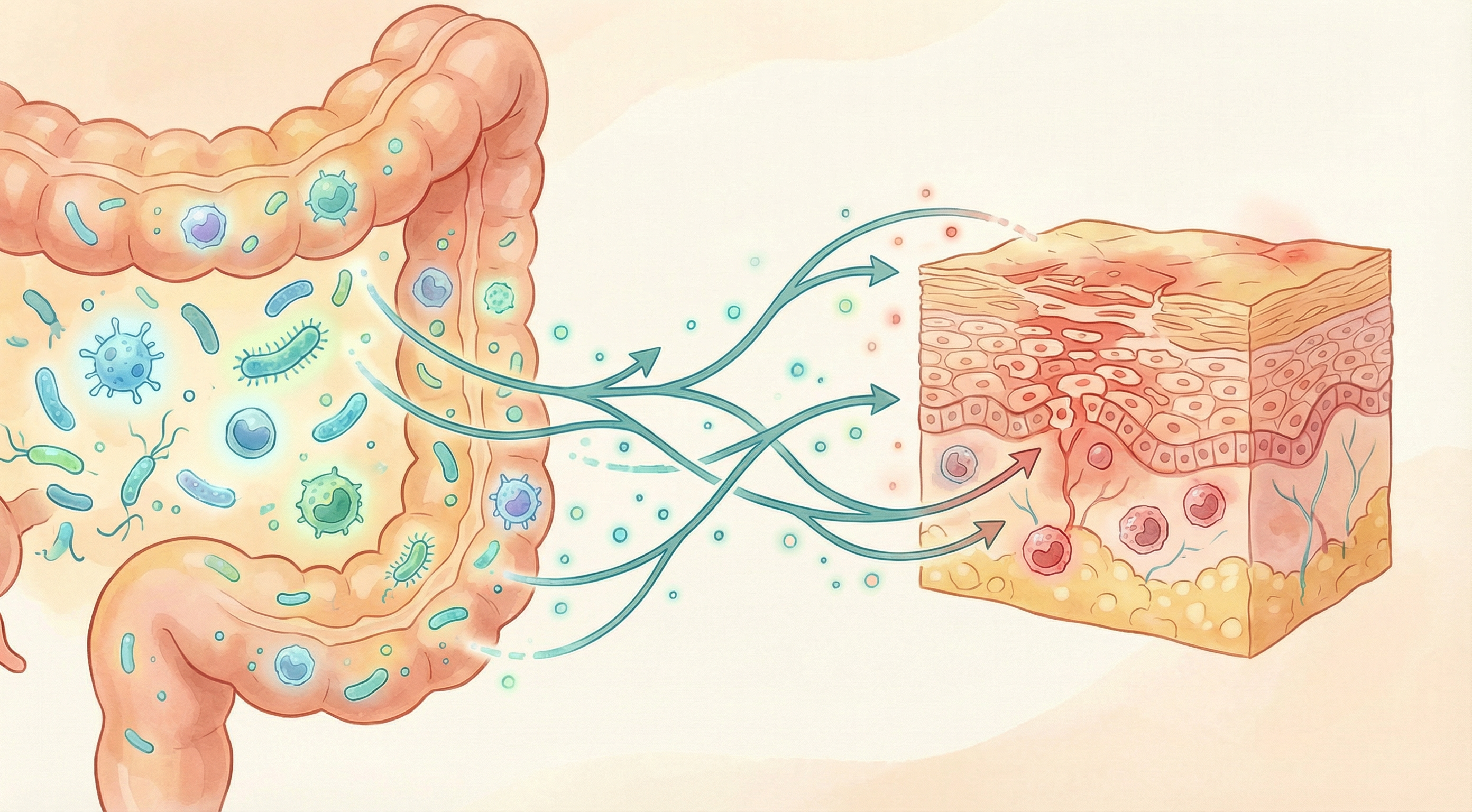
The Gut-Skin Axis in Eczema
Research has established a bidirectional communication pathway between the gut and skin—often called the "gut-skin axis." Microbial dysbiosis in both the skin and gut plays a critical role in the pathogenesis of atopic dermatitis, serving as a predictive biomarker for disease onset and a target for restorative therapeutic interventions.[2] This connection helps explain why gut microbiome imbalances can manifest as skin inflammation and why addressing gut health can improve skin conditions like eczema.
Early Life Microbiome
Studies show that reduced microbial diversity in early life and specific alterations (like decreased Bifidobacteria) are associated with increased eczema risk. Research reveals significant differences in the gut microbiota structure between children with atopic dermatitis and healthy controls, characterized by a reduction in microbial diversity and an increase in harmful bacteria.[3] Factors like C-section delivery, antibiotic use, and formula feeding can influence this risk.
Immune Development
The gut microbiome helps train the immune system in early life. Disruptions can lead to immune dysregulation, including the Th2-dominant immune responses characteristic of atopic conditions like eczema.
Intestinal Permeability
Increased intestinal permeability ("leaky gut") allows bacterial components and food allergens to enter circulation, potentially triggering systemic inflammation that can manifest in the skin.
Microbial Metabolites
Short-chain fatty acids (SCFAs) and other metabolites produced by gut bacteria have anti-inflammatory effects and help maintain skin barrier integrity. A significant association exists between gut microbiome dysbiosis, metabolic dysregulation, leaky gut, and the severity of atopic dermatitis.[4] Reduced SCFA production is observed in many eczema patients.
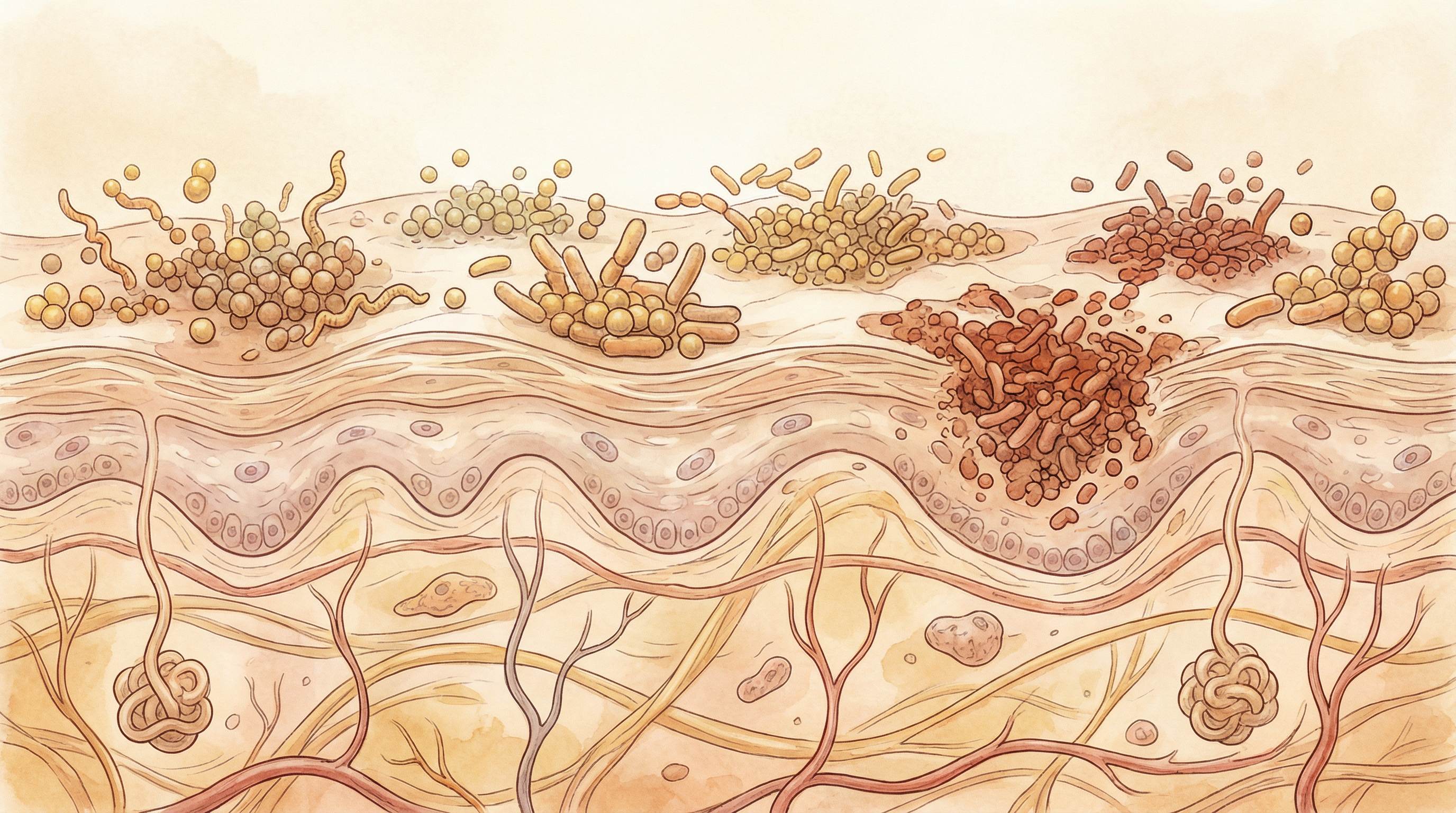
The Skin Microbiome in Eczema
The skin microbiome—the collection of microorganisms living on the skin surface—is dramatically altered in eczema, with these changes both resulting from and contributing to the condition:[5]
Staphylococcus aureus
Impact: Harmful, dramatically overgrown in eczema lesions Function: Produces toxins that damage the skin barrier, triggers inflammation, and inhibits antimicrobial peptide production[6]
Staphylococcus epidermidis
Impact: Beneficial, often depleted in eczema Function: Produces antimicrobial compounds that inhibit S. aureus growth and helps maintain skin barrier function[7]
Cutibacterium acnes
Impact: Beneficial, typically reduced in eczema Function: Produces short-chain fatty acids that maintain skin pH and inhibit pathogen growth
Malassezia species
Impact: Mixed; can trigger inflammation in some individuals Function: Normal skin commensal that can become problematic in certain contexts, particularly in seborrheic dermatitis
The hallmark of eczema is a dramatic increase in Staphylococcus aureus colonization, with up to 90% of eczema patients showing high levels of this bacterium on affected skin.[8] S. aureus produces various toxins and enzymes that damage the skin barrier, trigger inflammation, and create a vicious cycle of worsening symptoms.
Importantly, research shows that microbiome changes often precede visible eczema flares, suggesting that monitoring the skin microbiome could potentially predict and prevent flare-ups before they occur.[5]
Microbiome-Based Approaches for Eczema Management
Emerging research supports several microbiome-focused strategies for managing eczema symptoms:
Topical Probiotics
Creams and lotions containing beneficial bacteria like Staphylococcus epidermidis, Lactobacillus species, or Roseomonas mucosa can help restore skin microbiome balance and reduce S. aureus colonization.[7] Clinical trials have shown promising results with reduced inflammation and improved symptoms. Evidence Level: Moderate
Oral Probiotics
Specific probiotic strains, particularly Lactobacillus rhamnosus GG and Bifidobacterium species, have shown benefits in preventing and reducing eczema severity, especially when started early in life.[9] Effects appear to be strain-specific and may be more pronounced in children. Evidence Level: Moderate
Prebiotics
Dietary fibers that selectively feed beneficial bacteria can improve gut microbiome composition and reduce inflammation. Galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) have shown particular promise for eczema management. Evidence Level: Preliminary to Moderate
Dietary Modifications
Anti-inflammatory diets rich in omega-3 fatty acids, polyphenols, and fermented foods can positively influence both gut and skin microbiomes. Mediterranean and traditional Asian diets have been associated with lower eczema prevalence. Evidence Level: Preliminary
These microbiome-based approaches are most effective when integrated with conventional eczema management strategies, including appropriate moisturization, trigger avoidance, and medical treatments when necessary.

The Microbiome-Immune Connection in Eczema
The relationship between the microbiome and immune system is particularly relevant in eczema, which fundamentally involves immune dysregulation:
Key Microbiome-Immune Interactions in Eczema
- Regulatory T cells (Tregs) - Beneficial gut bacteria like Bifidobacteria promote Treg development, which helps prevent excessive immune responses
- Th1/Th2 balance - A healthy microbiome supports balanced Th1/Th2 responses, while dysbiosis can promote the Th2-dominant pattern seen in eczema
- Antimicrobial peptides - The microbiome influences production of these natural antibiotics that help control S. aureus colonization[7]
- Barrier function - Microbial metabolites like short-chain fatty acids help maintain both gut and skin barrier integrity
This complex interplay explains why approaches that target the microbiome can have profound effects on immune function and eczema symptoms, potentially addressing a root cause rather than just managing symptoms.
Clinical Evidence and Research Highlights
Recent studies have provided compelling evidence for the microbiome-eczema connection:
A landmark study in Science Translational Medicine found that S. epidermidis and other coagulase-negative staphylococci produce antimicrobial peptides that selectively kill S. aureus, and these protective bacteria are deficient in eczema patients.[7]
Research in Genome Research demonstrated that eczema flares are associated with increased S. aureus dominance and decreased bacterial diversity, with successful treatment restoring a more balanced microbiome.[5]
A systematic review and meta-analysis found that probiotic supplementation during pregnancy and early life reduces eczema risk by approximately 20% in at-risk children.[9]
Future Directions in Eczema Microbiome Research
The field of eczema microbiome research is rapidly evolving, with several promising directions:
Personalized Approaches
Research is increasingly focusing on identifying specific microbiome signatures that might predict response to different treatments, potentially enabling more personalized approaches to eczema management.
Novel Interventions
Beyond traditional probiotics, researchers are exploring next-generation approaches including:
- Engineered live biotherapeutics designed to target specific aspects of eczema pathophysiology
- Bacteriophages that selectively target S. aureus while preserving beneficial bacteria
- Postbiotics derived from beneficial microorganisms that may have direct anti-inflammatory effects
Prevention Strategies
Understanding the early-life microbiome factors that influence eczema development opens possibilities for prevention, particularly in high-risk infants with family history of atopic conditions.
The integration of microbiome science into eczema management represents a paradigm shift toward addressing underlying biological mechanisms rather than just managing symptoms. While much research remains to be done, the evidence to date suggests that nurturing healthy skin and gut microbiomes may be an important component of comprehensive eczema care.
Research Summary
Research has established a bidirectional communication pathway between the gut and skin—often called the 'gut-skin axis.' This connection helps explain why gut microbiome imbalances can manifest as skin inflammation and why addressing gut health can improve skin conditions like eczema.
References
- Wollina U.. Microbiome in atopic dermatitis. Clinical, Cosmetic and Investigational Dermatology. 2017;10:51-56. doi:10.2147/CCID.S130013 ↩
- Hou B, Shao H, Yuan D, Tham EH.. Skin and gut microbiome in atopic dermatitis: Mechanisms and therapeutic opportunities. Pediatric Allergy and Immunology. 2025;36(12):e70265. doi:10.1111/pai.70265 ↩
- Tang H, Li W, Xu Y, et al.. Gut microbiota modulation: a key determinant of atopic dermatitis susceptibility in children. Frontiers in Microbiology. 2025;16:1549895. doi:10.3389/fmicb.2025.1549895 ↩
- Blicharz L, Samborowska E, Zagożdżon R, et al.. Severity of atopic dermatitis is associated with gut-derived metabolites and leaky gut-related biomarkers. Scientific Reports. 2025;15:26146. doi:10.1038/s41598-025-09520-y ↩
- Kong HH, Oh J, Deming C, et al.. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Research. 2012;22(5):850-859. doi:10.1101/gr.131029.111 ↩
- Byrd AL, Deming C, Cassidy SKB, et al.. Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis. Science Translational Medicine. 2017;9(397):eaal4651. doi:10.1126/scitranslmed.aal4651 ↩
- Nakatsuji T, Chen TH, Narala S, et al.. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Science Translational Medicine. 2017;9(378):eaah4680. doi:10.1126/scitranslmed.aah4680 ↩
- Tao R, Li R, Wang R.. Skin microbiome alterations in atopic dermatitis patients. Annals of Dermatology. 2019;31(2):174-180. doi:10.5021/ad.2019.31.2.174 ↩
- Cuello-Garcia CA, Brożek JL, Fiocchi A, et al.. Probiotics for the prevention of allergy: A systematic review and meta-analysis of randomized controlled trials. Journal of Allergy and Clinical Immunology. 2015;136(4):952-961. doi:10.1016/j.jaci.2015.04.031 ↩
