The Gut-Brain Connection: How Your Microbiome Affects Mental Health
For decades, scientists focused on the brain as the primary control center for mental health. However, groundbreaking research over the past ten years has revealed a surprising player in mental wellbeing: the trillions of microorganisms residing in your gut[1].
The Bidirectional Highway: Understanding the Gut-Brain Axis
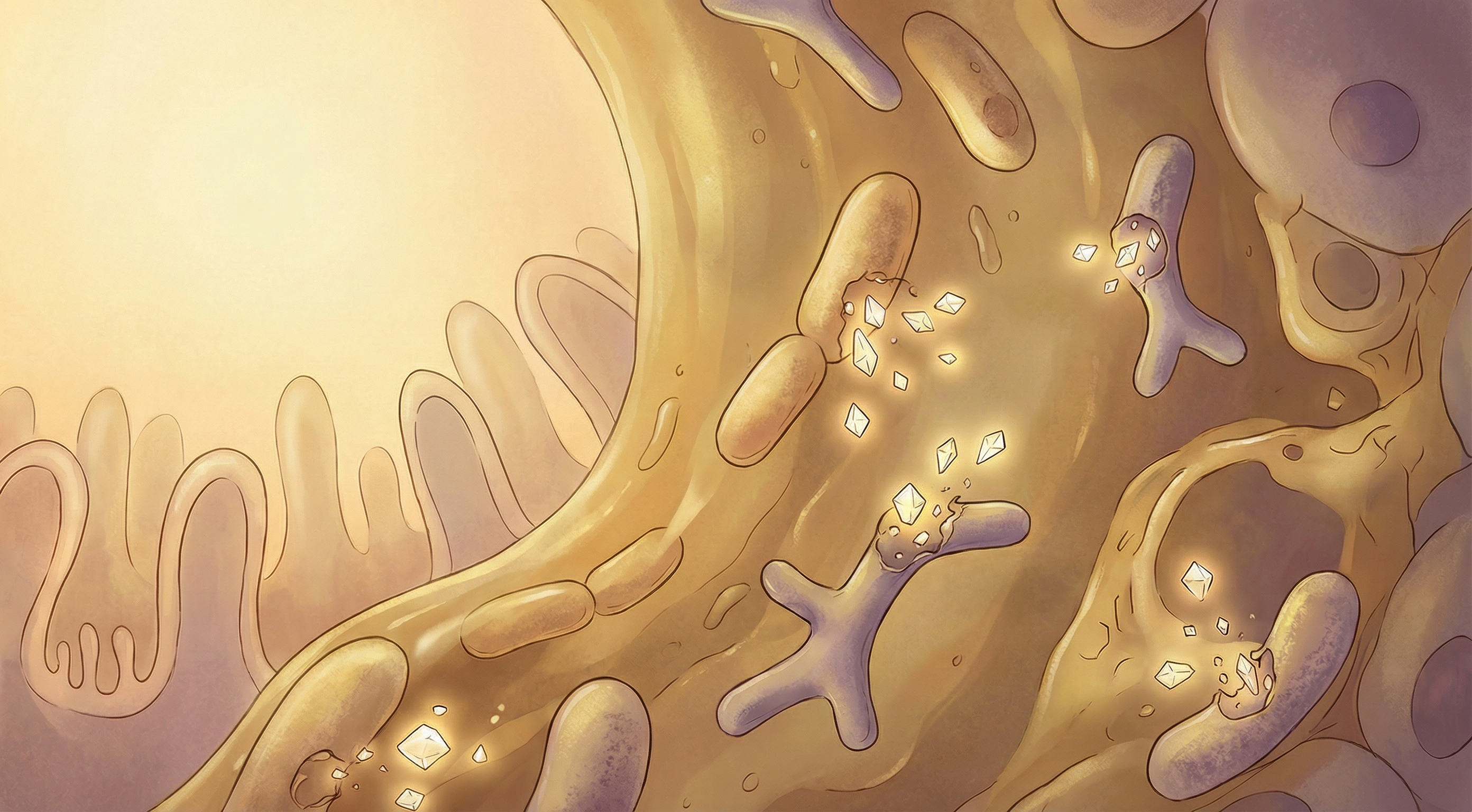
The gut-brain axis is a complex communication network connecting your central nervous system with your enteric nervous system—often called your "second brain." This bidirectional highway allows constant information exchange through several pathways[2]:
- Vagus Nerve Signaling: The vagus nerve serves as a direct communication line between gut bacteria and the brain, with approximately 80% of its fibers carrying signals from gut to brain[3].
- Immune System Mediation: Gut microbes influence systemic inflammation, which affects brain function.
- Neurotransmitter Production: Certain gut bacteria produce neurotransmitters like serotonin, GABA, and dopamine. Remarkably, about 95% of the body's serotonin is produced in the gut[4].
- Metabolite Signaling: Bacterial metabolites, particularly short-chain fatty acids, influence brain function and development.

Key Microbiome Players in Mental Health
Research has identified several microorganisms with significant impacts on mental health[5]:
Lactobacillus and Bifidobacterium Species
These beneficial bacteria have been extensively studied for their positive effects on mental health:
- Reduce anxiety and depression-like behaviors in animal models[3]
- Lower cortisol levels during stress
- Improve cognitive function and memory
- Enhance GABA production, promoting relaxation
Bacteroides fragilis
This commensal bacterium plays a crucial role in neurodevelopment[7]:
- Helps maintain proper blood-brain barrier function
- Reduces neuroinflammation
- May improve social behavior in autism spectrum disorders
- Produces important metabolites that influence brain development
Harmful Influences
Certain microbiome disruptions can negatively impact mental health:
- Pathogenic bacteria can increase inflammation, linked to depression
- Reduced microbiome diversity correlates with higher anxiety
- Certain bacterial overgrowths may contribute to brain fog and cognitive issues
Clinical Evidence: Microbiome Interventions for Mental Health
The growing body of research has led to several promising interventions:
Psychobiotics
Specific probiotic strains showing mental health benefits have been termed "psychobiotics"[6]:
- Lactobacillus rhamnosus has reduced anxiety in clinical trials, with effects mediated through the vagus nerve[3]
- Bifidobacterium longum has shown antidepressant effects comparable to pharmaceutical treatments in some studies
- Combination probiotics (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) have improved symptoms in patients with major depressive disorder[8]
Dietary Approaches
Nutrition strategies to support a mental health-promoting microbiome:
- Mediterranean diet rich in polyphenols and fiber
- Fermented foods like yogurt, kefir, and kimchi
- Prebiotic-rich foods that feed beneficial bacteria
- Omega-3 fatty acids to reduce neuroinflammation
Fecal Microbiota Transplantation
While still experimental for mental health conditions, early research shows promise:
- Case studies report improvement in treatment-resistant depression
- Ongoing clinical trials for autism spectrum disorders
- Potential applications for anxiety disorders
Future Directions in Microbiome-Based Mental Health Care
The field is rapidly evolving with several exciting developments on the horizon[1]:
- Personalized Microbiome Analysis: Tailoring interventions based on individual microbiome profiles
- Targeted Psychobiotics: Developing specific bacterial strains engineered to produce neuroactive compounds
- Microbiome-Friendly Medications: Creating psychiatric medications that preserve microbiome health
- Integrated Treatment Approaches: Combining traditional psychiatric care with microbiome interventions
Practical Steps for Supporting Your Gut-Brain Health
While research continues, there are evidence-based steps you can take today:
- Diversify Your Diet: Aim for 30+ different plant foods weekly to support microbiome diversity
- Include Fermented Foods: Add yogurt, kefir, sauerkraut, or kimchi to your regular diet
- Prioritize Fiber: Consume prebiotic-rich foods like garlic, onions, leeks, asparagus, and bananas
- Reduce Ultra-Processed Foods: Minimize artificial sweeteners and emulsifiers that can disrupt gut bacteria
- Manage Stress: Practice stress-reduction techniques, as chronic stress negatively impacts the microbiome
- Consider Evidence-Based Probiotics: Consult healthcare providers about specific strains with mental health benefits[6]
The gut-brain connection represents one of the most exciting frontiers in mental health research. By understanding and nurturing our microbiome, we may unlock new approaches to treating and preventing mental health conditions that affect millions worldwide.

References
- Cryan JF, O'Riordan KJ, Cowan CSM, et al.. The Microbiota-Gut-Brain Axis. Physiological Reviews. 2019;99(4):1877-2013. doi:10.1152/physrev.00018.2018
- Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Journal of Clinical Investigation. 2015;125(3):926-938. doi:10.1172/JCI76304
- Bravo JA, Forsythe P, Chew MV, et al.. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences. 2011;108(38):16050-16055. doi:10.1073/pnas.1102999108
- Yano JM, Yu K, Donaldson GP, et al.. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015;161(2):264-276. doi:10.1016/j.cell.2015.02.047
- Dinan TG, Cryan JF. Gut instincts: microbiota as a key regulator of brain development, ageing, and neurodegeneration. The Journal of Physiology. 2017;595(2):489-503. doi:10.1113/JP273106
- Sarkar A, Lehto SM, Harty S, et al.. Psychobiotics and the Manipulation of Bacteria-Gut-Brain Signals. Trends in Neurosciences. 2016;39(11):763-781. doi:10.1016/j.tins.2016.09.002
- Hsiao EY, McBride SW, Hsien S, et al.. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013;155(7):1451-1463. doi:10.1016/j.cell.2013.11.024
- Messaoudi M, Lalonde R, Violle N, et al.. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. British Journal of Nutrition. 2011;105(5):755-764. doi:10.1017/S0007114510004319
