Better Cortisol Regulation
Optimize your body's stress hormone response through gut microbiome support for improved energy, sleep, and overall wellbeing.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
Cortisol: The Misunderstood Hormone
Cortisol is often called the "stress hormone," but it's essential for life. It helps you wake up in the morning, respond to challenges, regulate blood sugar, and control inflammation. The problem isn't cortisol itself—it's dysregulated cortisol that causes issues.[1]
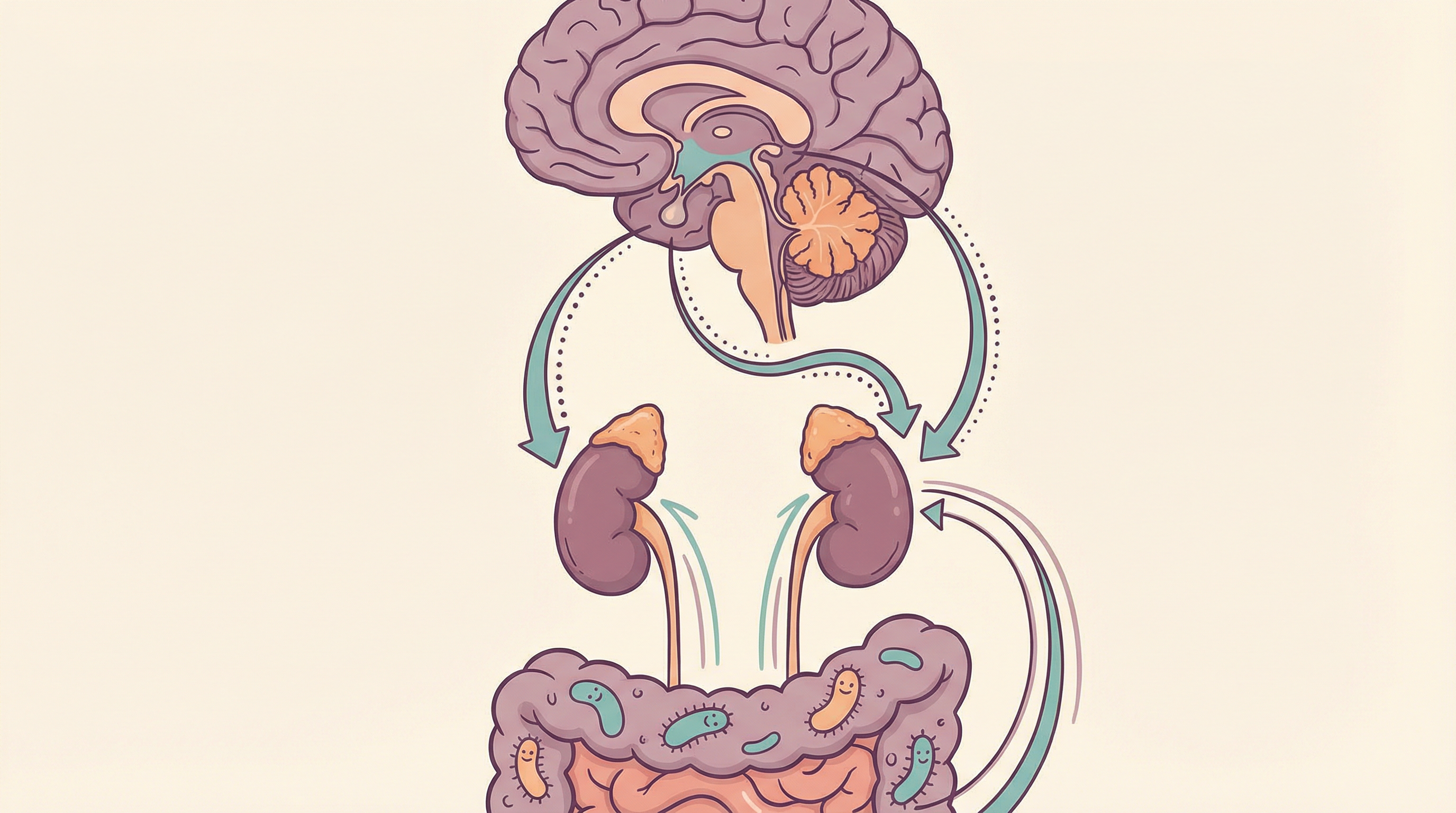
What's fascinating is that your gut microbiome has profound influence over how your body produces, responds to, and recovers from cortisol. This gut-HPA axis connection offers new approaches to managing stress and optimizing energy.
The HPA Axis and Microbiome Connection
How the Stress Response Works
The hypothalamic-pituitary-adrenal (HPA) axis controls cortisol:
Normal stress response:
- Brain perceives stressor
- Hypothalamus releases CRH
- Pituitary releases ACTH
- Adrenal glands release cortisol
- Cortisol helps you cope with the challenge
- Feedback mechanisms shut down the response
Healthy cortisol rhythm:
- Highest in the morning (cortisol awakening response)
- Gradually decreases through day
- Lowest at bedtime
- Allows for alert days and restful nights
How Gut Bacteria Influence Cortisol
Research shows the microbiome shapes HPA axis development and function:[1]
Early programming:
- Germ-free animals have exaggerated stress responses
- Early-life microbiome shapes lifelong HPA function
- Colonization with beneficial bacteria normalizes responses
Ongoing regulation:
- Bacterial metabolites affect brain stress circuitry
- Inflammation from dysbiosis activates HPA axis
- Beneficial bacteria can dampen excessive responses
- Vagus nerve mediates gut-brain stress communication
The Vicious Cycle
Stress and gut health create feedback loops:[2]
Stress damages the gut:
- Increases intestinal permeability
- Alters microbiome composition
- Reduces beneficial bacteria
- Increases inflammatory species
Gut problems increase stress response:
- Inflammation activates HPA axis
- Dysbiosis may cause anxiety and mood issues
- Poor gut-brain signaling
- Cycle perpetuates itself
Signs of Cortisol Dysregulation
Chronically High Cortisol
- Difficulty falling asleep
- Waking between 2-4 AM
- Anxiety and racing thoughts
- Weight gain, especially abdominal
- Blood sugar swings
- High blood pressure
- Weakened immune function
- Memory problems
Low Cortisol (Burnout Pattern)
- Difficulty waking up
- Fatigue throughout the day
- Craving salt or sugar
- Low blood pressure
- Dizziness upon standing
- Feeling overwhelmed by minor stress
- Frequent illness
- Low motivation
Disrupted Rhythm
- Energy fluctuations throughout day
- "Second wind" at night
- Feeling tired but wired
- Sleep that's not restorative
Key Microbes for Cortisol Regulation
Lactobacillus rhamnosus
Most studied for stress reduction:
- Reduces cortisol response to stress
- Effects mediated by vagus nerve
- Strain JB-1 particularly researched
- Reduces anxiety behaviors
Bifidobacterium longum
Specifically affects cortisol:[3]
- Strain 1714 reduces cortisol awakening response
- Improves cognitive performance under stress
- Reduces subjective stress
- Well-tolerated in human trials
Lactobacillus helveticus
Often combined with B. longum:
- Combination reduces cortisol
- Improves anxiety and depression scores
- Effects seen in healthy volunteers
- Part of well-studied psychobiotic formulation
Lactobacillus plantarum
Supports stress resilience:
- Reduces stress-related markers
- Supports gut barrier under stress
- May protect against stress-induced dysbiosis
- Multiple strains show benefits
Dietary Strategies for Cortisol Balance
Blood Sugar Stability
Blood sugar swings trigger cortisol:
Do:
- Eat regular meals
- Include protein with each meal
- Choose complex carbohydrates
- Include healthy fats
- Avoid skipping breakfast
Avoid:
- Large amounts of sugar
- Refined carbohydrates alone
- Long gaps without eating
- Excessive caffeine on empty stomach
Cortisol-Supporting Nutrients
Vitamin C:
- Adrenal glands store vitamin C
- Used during cortisol production
- Citrus, bell peppers, broccoli
- May blunt cortisol response to stress
Magnesium:
- Calms HPA axis
- Often depleted by stress
- Leafy greens, nuts, dark chocolate
- Consider supplementation if deficient
B vitamins:
- Support adrenal function
- Used in stress response
- Whole grains, legumes, eggs
- B5 particularly important for adrenals
Omega-3 fatty acids:
- Reduce inflammation
- May modulate cortisol response
- Fatty fish, walnuts, flaxseed
Adaptogenic Herbs
Herbs that help regulate stress response:
Ashwagandha:
- Reduces cortisol levels
- Improves stress resilience
- Well-studied adaptogen
- Start with low dose
Rhodiola:
- Helps with fatigue
- May lower cortisol
- Supports mental performance under stress
Holy basil:
- Traditional stress remedy
- May help normalize cortisol
- Can be enjoyed as tea
Fermented Foods
Support gut-brain stress communication:
- Daily consumption recommended
- Variety of types
- Choose unpasteurized when possible

Lifestyle Factors
Sleep Hygiene
Critical for cortisol rhythm:
- Consistent sleep/wake times
- Dark room for sleeping
- Avoid screens before bed
- Avoid late-night eating
- Address sleep disorders
Stress Management Practices
Direct cortisol-lowering effects:
- Meditation (even 10 minutes helps)
- Deep breathing exercises
- Yoga
- Time in nature
- Social connection
Exercise
Affects cortisol in complex ways:
- Regular moderate exercise lowers baseline cortisol
- Intense exercise temporarily raises cortisol
- Balance intensity with recovery
- Morning exercise supports natural cortisol rhythm
Caffeine
Caffeine increases cortisol:
- Limit especially if anxious or sleep-disrupted
- Avoid after noon
- Some people more sensitive
- May need to reduce or eliminate
Light Exposure
Light affects cortisol rhythm:
- Morning bright light supports healthy awakening response
- Reduce blue light in evening
- Natural light exposure beneficial
- Consider light therapy in winter

Testing Cortisol
If concerned about cortisol:
Salivary cortisol:
- Multiple samples throughout day
- Shows rhythm pattern
- Non-invasive
- DUTCH test is comprehensive option
Blood cortisol:
- Single point in time
- Less informative about rhythm
- May be elevated from stress of blood draw
Building Better Cortisol Regulation
Supporting cortisol balance through the microbiome involves:
- Supporting beneficial bacteria with psychobiotics and fermented foods
- Stabilizing blood sugar with regular, balanced meals
- Managing stress actively with daily practices
- Prioritizing sleep for healthy cortisol rhythm
- Including adaptogens and nutrients that support adrenal function
- Breaking the stress-gut cycle with comprehensive approach
Most people notice improvements in energy and stress tolerance within 3-4 weeks of consistent gut-HPA support. Fully restoring healthy cortisol patterns may take 2-3 months, especially if coming from a state of chronic stress or burnout.
Supporting Practices
Evidence-based strategies to support this benefit:
- Practice regular meditation or deep breathing
- Maintain consistent sleep and wake times
- Include adaptogenic herbs like ashwagandha and rhodiola
- Eat regular, balanced meals to stabilize blood sugar
- Limit caffeine, especially after noon
- Engage in regular moderate exercise
References
- Sudo N, Chida Y, Aiba Y, et al.. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. Journal of Physiology. 2004;558(Pt 1):263-275. doi:10.1113/jphysiol.2004.063388 ↩
- Karl JP, Margolis LM, Madslien EH, et al.. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. American Journal of Physiology. 2017;312(6):G559-G571. doi:10.1152/ajpgi.00066.2017 ↩
- Allen AP, Hutch W, Borre YE, et al.. Bifidobacterium longum 1714 as a translational psychobiotic: modulation of stress, electrophysiology and neurocognition in healthy volunteers. Translational Psychiatry. 2016;6(11):e939. doi:10.1038/tp.2016.191 ↩
