Optimized Estrogen Metabolism
Support healthy estrogen levels and metabolism through the gut microbiome's estrobolome for hormonal balance and reduced disease risk.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Estrobolome: Your Gut's Hormone Regulator
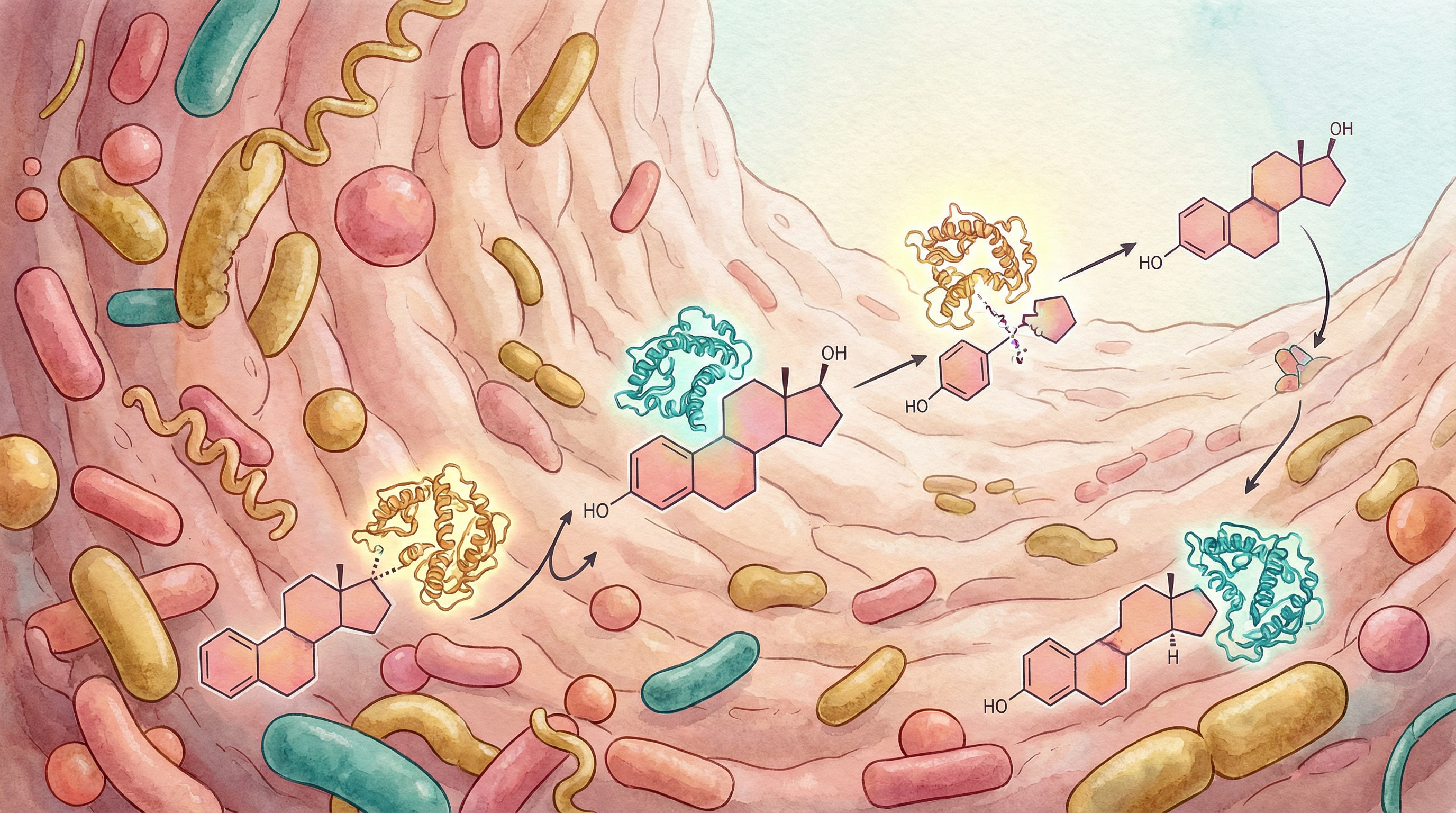
Within your gut microbiome exists a specialized collection of bacteria that specifically metabolize estrogen—collectively called the "estrobolome." This bacterial community plays a crucial role in determining how much estrogen circulates in your body and how effectively it's processed and eliminated.[1]
Understanding and supporting your estrobolome is essential for hormonal health, affecting everything from menstrual regularity to long-term disease risk.
How the Estrobolome Works
The Estrogen Lifecycle
Estrogen goes through a complex journey:[2]
Production:
- Ovaries (primarily in premenopausal women)
- Adrenal glands
- Fat tissue (becomes more important after menopause)
Liver processing:
- Estrogen is metabolized in the liver
- Conjugated (attached to glucuronic acid)
- Conjugated estrogen is water-soluble and ready for excretion
Gut excretion (or recycling):
- Conjugated estrogen enters gut via bile
- Here's where the estrobolome matters:
- Bacteria with beta-glucuronidase can deconjugate estrogen
- Deconjugated (free) estrogen can be reabsorbed
- This recycles estrogen back into circulation
- Or, estrogen continues to be excreted in stool
Beta-Glucuronidase: The Key Enzyme
This bacterial enzyme determines estrogen fate:
High beta-glucuronidase activity:
- More estrogen is deconjugated
- More estrogen recirculates
- Can lead to estrogen excess
- Associated with certain health risks
Low/balanced beta-glucuronidase activity:
- More estrogen is excreted
- Healthy estrogen levels maintained
- Reduced risk of estrogen-related conditions
Which Bacteria Have Beta-Glucuronidase?
Over 60 bacterial species produce this enzyme:
- Certain Clostridium species
- Some Bacteroides species
- Various Escherichia species
- Some Lactobacillus and Bifidobacterium (usually lower levels)
The overall balance of your microbiome determines net beta-glucuronidase activity.

Why Estrogen Balance Matters
Too Much Estrogen (Estrogen Dominance)
Can contribute to:[3]
- PMS symptoms
- Heavy, painful periods
- Fibroids
- Endometriosis
- Certain breast cancers
- Weight gain, especially hips and thighs
- Mood swings and anxiety
Too Little Estrogen
Can contribute to:
- Menopausal symptoms (hot flashes, vaginal dryness)
- Bone loss and osteoporosis
- Cognitive changes
- Cardiovascular changes
- Mood disturbances
The Goal: Balance
Optimal estrogen metabolism maintains:
- Appropriate levels for your life stage
- Efficient clearance of estrogen metabolites
- Balance between different estrogen forms
- Reduced risk of estrogen-related diseases
Signs of Estrogen Imbalance
Possible estrogen excess:
- Heavy or prolonged periods
- Breast tenderness or swelling
- Weight gain (hips/thighs)
- Mood swings before period
- Fibrocystic breasts
- Fibroids
Possible estrogen deficiency:
- Hot flashes and night sweats
- Vaginal dryness
- Decreased libido
- Sleep disturbances
- Joint pain
- Brain fog
Dietary Strategies for Estrogen Balance
Support Healthy Estrogen Metabolism
Cruciferous vegetables:
- Broccoli, cauliflower, Brussels sprouts, kale
- Contain indole-3-carbinol and DIM
- Support healthy estrogen metabolite ratios
- Aim for daily consumption
Fiber:
- Essential for estrogen excretion
- Reduces enterohepatic recycling
- Diverse fiber types best
- Aim for 25-35g daily
Ground flaxseed:
- Contains lignans (phytoestrogens)
- May help modulate estrogen activity
- Provides fiber
- 1-2 tablespoons daily
Support Healthy Microbiome
Fermented foods:
- Support diverse, balanced microbiome
- Include daily
- Variety of fermented foods
Prebiotic fibers:
- Feed beneficial bacteria
- May help balance beta-glucuronidase activity
- Diverse plant foods
Foods to Limit
Alcohol:
- Increases estrogen levels
- Impairs liver estrogen metabolism
- Even moderate intake has effects
- Limit or avoid
Excessive red meat:
- Associated with higher estrogen levels
- Moderate consumption
- Choose quality sources
Processed foods:
- May contain xenoestrogens
- Disrupt microbiome
- Limit overall intake

Lifestyle Factors
Maintain Healthy Weight
Fat tissue produces estrogen:
- Excess body fat means excess estrogen
- Weight loss can help estrogen excess
- Microbiome affects weight management
- Sustainable approach is best
Exercise
Physical activity supports estrogen balance:
- Helps maintain healthy weight
- May improve estrogen metabolism
- Supports healthy microbiome
- Regular, moderate activity
Reduce Xenoestrogen Exposure
Environmental chemicals can mimic estrogen:
- BPA in plastics
- Parabens in personal care products
- Pesticides on produce
- Choose glass/stainless over plastic
- Select cleaner personal care products
- Choose organic when possible (especially dirty dozen)
Stress Management
Chronic stress affects hormones:
- Affects cortisol which interacts with estrogen
- May disrupt microbiome
- Can worsen hormonal symptoms
- Regular stress reduction practices help
Sleep
Adequate sleep supports hormonal balance:
- Hormone production follows circadian rhythms
- Poor sleep disrupts hormonal cycles
- Prioritize consistent, quality sleep
Special Considerations
Menopause
The estrobolome becomes more important:
- Ovarian estrogen production declines
- Estrobolome affects remaining estrogen levels
- May influence severity of symptoms
- Supporting gut health can help transition
Breast Cancer Risk
Estrobolome affects risk:[3]
- Certain microbiome patterns associated with increased risk
- Healthy estrogen metabolism may be protective
- Discuss with healthcare provider if high risk
- Lifestyle factors can help
Hormone Replacement Therapy
If using HRT:
- Oral estrogen goes through gut
- Estrobolome affects metabolism
- Gut health may affect HRT effectiveness
- Transdermal bypasses gut
Testing
Consider testing if concerned:
- Estrogen metabolite testing (DUTCH test)
- Microbiome testing
- Hormone panels
- Work with knowledgeable practitioner
Building Better Estrogen Balance
Supporting estrogen metabolism through the estrobolome involves:
- Eating cruciferous vegetables daily
- Increasing fiber intake for proper excretion
- Supporting beneficial bacteria with fermented foods
- Maintaining healthy weight through diet and exercise
- Reducing xenoestrogen exposure in products and food
- Managing stress and sleep for overall hormonal support
Most people notice improvements in hormonal symptoms within 1-2 menstrual cycles (4-8 weeks). Fully optimizing estrogen metabolism through the estrobolome is an ongoing process that improves steadily with consistent lifestyle practices.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume cruciferous vegetables for healthy estrogen metabolism
- Include fiber to support estrogen excretion
- Limit alcohol which affects estrogen levels
- Maintain healthy weight for optimal hormone balance
- Choose organic produce when possible to reduce xenoestrogen exposure
- Include fermented foods to support estrobolome bacteria
References
- Plottel CS, Blaser MJ. Microbiome and malignancy. Cell Host & Microbe. 2011;10(4):324-335. doi:10.1016/j.chom.2011.10.003 ↩
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017;103:45-53. doi:10.1016/j.maturitas.2017.06.025 ↩
- Kwa M, Plottel CS, Blaser MJ, Adams S. The intestinal microbiome and estrogen receptor-positive female breast cancer. Journal of the National Cancer Institute. 2016;108(8):djw029. doi:10.1093/jnci/djw029 ↩
