Improved Thyroid Conversion
Support healthy thyroid hormone conversion and function through gut microbiome optimization for better metabolism and energy.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Gut-Thyroid Connection
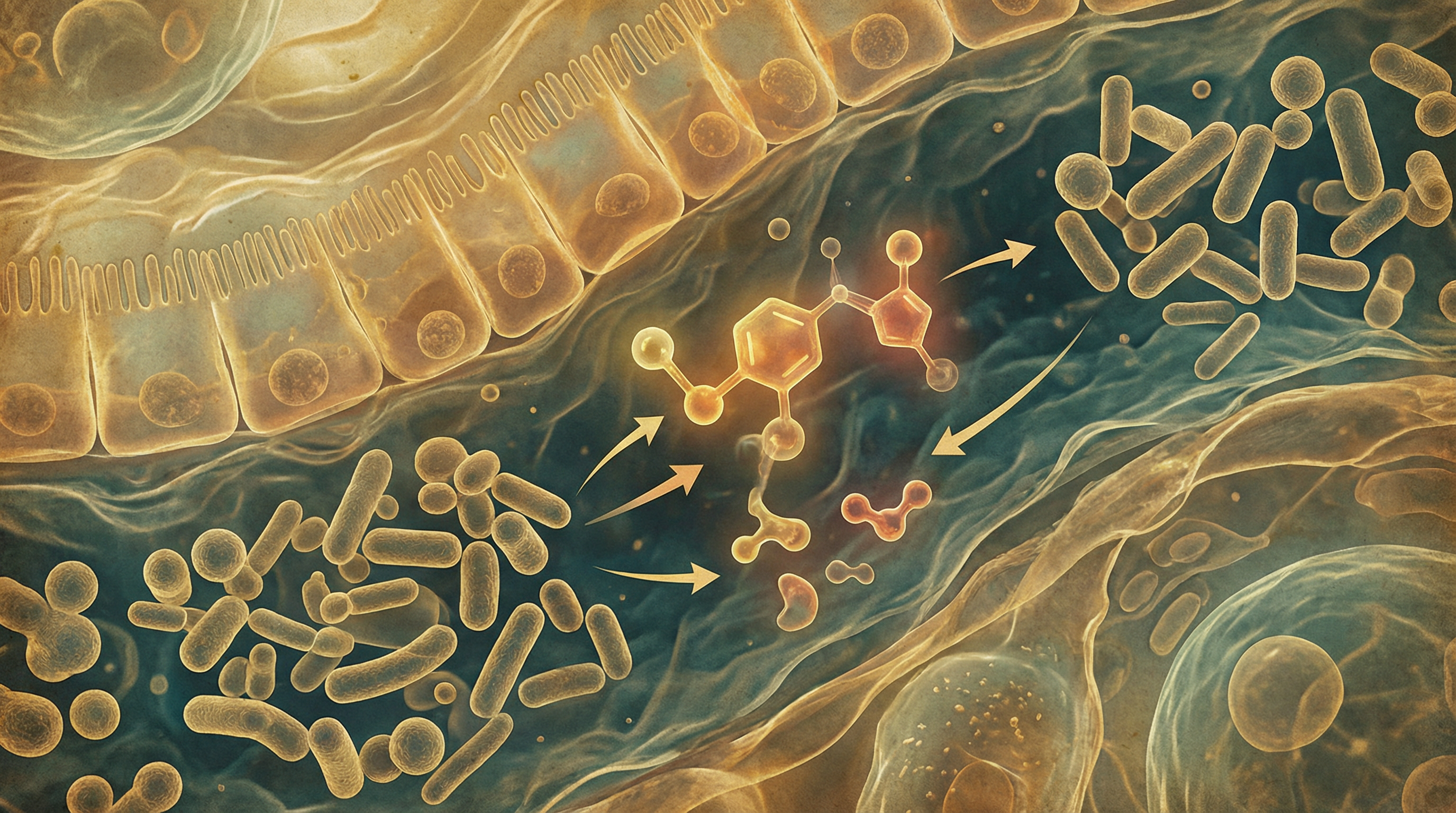
Your thyroid gland is the master regulator of metabolism, affecting everything from energy levels to body temperature to weight. But thyroid function isn't just about the thyroid itself—your gut microbiome plays a significant role in thyroid hormone activation, nutrient absorption, and immune regulation that affects thyroid health.[1]
Understanding this gut-thyroid axis reveals new approaches to supporting optimal thyroid function.
How the Gut Affects Thyroid Function
Hormone Conversion
The thyroid produces mostly T4 (inactive form), which must be converted to T3 (active form):[2]
Where conversion happens:
- About 20% in the gut
- Also in liver, kidneys, and other tissues
- Gut bacteria directly participate in this conversion
- Healthy microbiome supports efficient conversion
Bacterial influence:
- Some bacteria have deiodinase-like enzymes
- May directly convert T4 to T3
- Dysbiosis may impair this conversion
- Contributing to low T3 despite normal T4
Nutrient Absorption
Key thyroid nutrients depend on gut health:
Selenium:
- Essential for conversion enzymes (deiodinases)
- Absorption requires healthy gut
- Brazil nuts are richest food source
- Deficiency impairs T4 to T3 conversion
Zinc:
- Required for thyroid hormone synthesis and conversion
- Absorption gut-dependent
- Deficiency common in gut disorders
- Also needed for TSH production
Iodine:
- Building block of thyroid hormones
- Absorption can be affected by gut issues
- Found in seaweed, seafood, iodized salt
- Both deficiency and excess problematic
Iron:
- Needed for thyroid hormone synthesis
- Often malabsorbed with gut problems
- Common deficiency in hypothyroidism
- Check ferritin levels
Immune Modulation
Most thyroid problems are autoimmune:[3]
Hashimoto's thyroiditis:
- Most common cause of hypothyroidism
- Immune system attacks thyroid
- Gut bacteria shape immune responses
- Dysbiosis may trigger or worsen autoimmunity
Graves' disease:
- Causes hyperthyroidism
- Also autoimmune in nature
- Gut health affects disease course
- Some patients have distinct microbiome patterns
Molecular mimicry:
- Some gut bacteria have proteins similar to thyroid tissue
- May trigger cross-reactive immune responses
- LPS from leaky gut increases inflammation
- Healing gut may help autoimmunity
LPS and Thyroid Function
Bacterial lipopolysaccharide (LPS) affects thyroid:
- Reduces T4 to T3 conversion
- Increases reverse T3 (inactive)
- Contributes to "sick euthyroid" pattern
- Gut permeability allows LPS into circulation

Signs of Thyroid Issues
Hypothyroidism (low thyroid)
- Fatigue and low energy
- Weight gain or difficulty losing weight
- Cold intolerance
- Dry skin and hair
- Constipation
- Depression
- Brain fog
- Slow heart rate
Hyperthyroidism (high thyroid)
- Weight loss despite eating
- Rapid heartbeat
- Anxiety and nervousness
- Heat intolerance
- Tremors
- Sleep difficulties
- Diarrhea
Key Microbiome Patterns in Thyroid Disorders
Research shows characteristic changes:[3]
In Hashimoto's:
- Reduced bacterial diversity
- Altered Lactobacillus populations
- Changes in Bifidobacterium
- Increased intestinal permeability
Common findings in thyroid patients:
- SIBO (small intestinal bacterial overgrowth) more common
- H. pylori infection more prevalent
- Dysbiosis patterns vary
- Gut symptoms often accompany thyroid issues
Dietary Strategies for Thyroid Support
Thyroid-Supporting Nutrients
Selenium sources:
- Brazil nuts (1-2 daily provides selenium)
- Fish and shellfish
- Eggs
- Don't over-supplement (toxicity possible)
Zinc sources:
- Pumpkin seeds
- Beef
- Chickpeas
- Oysters
Iodine sources (moderate amounts):
- Seaweed (small amounts)
- Fish and shellfish
- Iodized salt
- Avoid excessive intake
Iron sources:
- Red meat
- Legumes
- Leafy greens
- Pair with vitamin C for absorption
Support Gut Health
Fermented foods:
- Support beneficial bacteria
- May help autoimmune regulation
- Include regularly
Fiber:
- Supports healthy microbiome
- Helps with constipation (common in hypothyroidism)
- Diverse plant fibers
Bone broth:
- Supports gut healing
- Contains minerals
- May help with leaky gut
Foods to Consider Limiting
Gluten (for some people):
- Cross-reactivity with thyroid tissue proposed
- Autoimmune thyroid patients may benefit from trial elimination
- Not everyone needs to avoid
- Discuss with healthcare provider
Excessive raw cruciferous:
- Can interfere with iodine uptake in large amounts
- Cooking reduces this effect
- Moderate amounts fine for most
- Not a concern with adequate iodine
Soy (excessive amounts):
- May interfere with thyroid hormone absorption
- Moderate amounts generally fine
- Separate from thyroid medication by 4 hours

Lifestyle Factors
Stress Management
Stress significantly affects thyroid:
- Cortisol inhibits T4 to T3 conversion
- Increases reverse T3
- Worsens autoimmune conditions
- Regular stress reduction essential
Sleep
Sleep affects thyroid function:
- TSH follows circadian rhythm
- Sleep deprivation affects thyroid hormones
- Prioritize consistent, quality sleep
- Address sleep issues
Exercise
Physical activity supports thyroid:
- Improves thyroid sensitivity
- Supports healthy weight
- Beneficial for gut microbiome
- Moderate, regular exercise best
Avoid Toxins
Environmental factors affect thyroid:
- Reduce plastic exposure
- Filter water
- Choose clean personal care products
- Pesticide exposure may affect thyroid
Thyroid Medication and Gut Health
If taking thyroid medication:
Absorption matters:
- Medication absorption depends on gut health
- Take on empty stomach
- Separate from calcium, iron, fiber supplements
- Consistency important
Monitor and adjust:
- Improving gut health may affect medication needs
- May need dose adjustments
- Work with healthcare provider
- Regular monitoring important
Testing
Comprehensive thyroid evaluation:
- TSH (pituitary signal to thyroid)
- Free T4 (inactive hormone)
- Free T3 (active hormone)
- Reverse T3 (inactive metabolite)
- Thyroid antibodies (for autoimmunity)
- Consider microbiome testing
Building Better Thyroid Function
Supporting thyroid conversion through the gut involves:
- Ensuring adequate selenium and zinc from food
- Healing gut permeability to reduce LPS exposure
- Supporting beneficial bacteria with fiber and fermented foods
- Managing stress which impairs conversion
- Addressing potential food sensitivities (gluten trial if autoimmune)
- Working with healthcare provider for proper testing and monitoring
Most people notice improvements in energy and thyroid symptoms within 6-12 weeks of comprehensive gut-thyroid support. Full optimization is an ongoing process that requires consistent attention to gut health alongside conventional thyroid management.
Supporting Practices
Evidence-based strategies to support this benefit:
- Ensure adequate selenium intake from Brazil nuts and fish
- Include zinc-rich foods for thyroid enzyme function
- Manage stress which impairs thyroid conversion
- Support gut health to reduce thyroid autoimmunity
- Include iodine from seaweed and seafood (moderate amounts)
- Address gut inflammation that affects thyroid function
References
- Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function?. Nutrients. 2020;12(6):1769. doi:10.3390/nu12061769 ↩
- Virili C, Centanni M. Does microbiota composition affect thyroid homeostasis?. Endocrine. 2018;49(3):583-587. doi:10.1007/s12020-014-0509-2 ↩
- Zhao F, Feng J, Li J, et al.. Alterations of the Gut Microbiota in Hashimoto's Thyroiditis Patients. Thyroid. 2018;28(2):175-186. doi:10.1089/thy.2017.0395 ↩
