Better Appetite Signaling
Restore natural hunger and satiety cues through microbiome optimization for intuitive eating and healthy weight management.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
When Hunger Signals Go Wrong
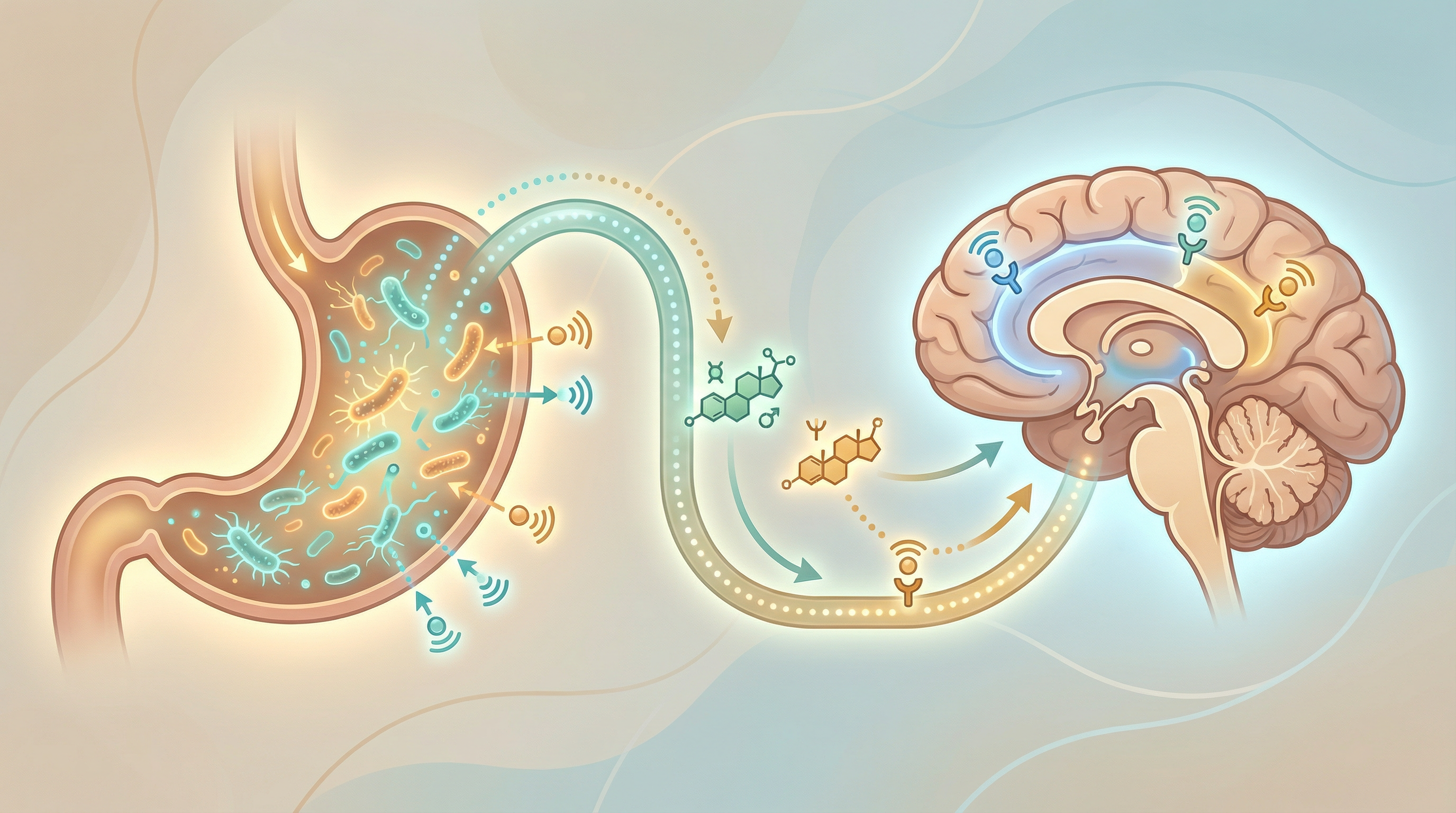
In an ideal world, hunger and fullness signals would guide us to eat exactly what we need—no more, no less. But modern diets, stress, and lifestyle factors have disrupted these ancient signaling systems for many people, leading to overeating, constant cravings, and difficulty maintaining healthy weight[1]. Emerging evidence even suggests that gut bacteria may actively manipulate host eating behavior to promote their own fitness, potentially contributing to cravings and food preferences[4].
What's become clear is that your gut microbiome is a central regulator of these signals. Bacteria don't just passively digest your food—they actively communicate with your brain about hunger and satiety.
How Bacteria Control Appetite
Hormone Production and Regulation
Gut bacteria influence key appetite hormones:
GLP-1 (Glucagon-like peptide-1):
- Powerful satiety signal
- Released by L-cells in the gut
- SCFAs from bacterial fermentation stimulate GLP-1 release
- GLP-1 drugs (like Ozempic) mimic this effect pharmaceutically
PYY (Peptide YY):
- Reduces appetite after meals
- Also stimulated by SCFAs
- Higher fiber intake increases PYY response
- Signals fullness to the brain
Ghrelin:
- The "hunger hormone"
- Some bacteria may affect ghrelin production
- Imbalanced microbiome may increase ghrelin
- Fiber intake helps regulate ghrelin
Leptin:
- Signals energy sufficiency
- Leptin resistance common in obesity
- Microbiome-driven inflammation contributes to resistance
- Healthy microbiome may improve leptin sensitivity
Direct Brain Communication
Bacteria communicate with the brain via the vagus nerve[3]. This microbiota-gut-brain axis plays a central role in appetite regulation and obesity[5]:
Bacterial proteins:
- Some bacteria produce proteins that mimic satiety hormones
- E. coli ClpB protein activates satiety pathways
- This provides an additional layer of appetite regulation
- May explain why microbiome composition affects food intake
Metabolite signaling:
- SCFAs directly affect brain appetite centers
- Reach the brain via circulation
- Influence hypothalamic function
- Provide feedback about gut nutrient status
Bacterial Growth Dynamics
Bacteria influence appetite through their own growth patterns:
Post-meal bacterial bloom:
- Bacteria multiply when nutrients arrive
- Stationary phase bacteria produce different signals
- This may contribute to meal-ending satiety
- Timing of bacterial growth affects appetite
Competition for nutrients:
- Some bacteria may increase host appetite to feed themselves
- Others may reduce appetite when satisfied
- The balance affects overall food-seeking behavior
Key Appetite-Regulating Microbes
Akkermansia muciniphila
Consistently associated with healthy appetite:
- Abundant in lean individuals
- May improve leptin and insulin signaling
- Supports gut barrier, reducing inflammation
- Responds to polyphenol-rich foods
Hafnia alvei
Novel probiotic for appetite control[2]:
- Produces ClpB protein that mimics satiety signals
- Reduced food intake in animal studies
- Being developed as a weight management probiotic
- Shows promise for appetite regulation
Bifidobacterium animalis
Supports healthy appetite signaling:
- Strain BB-12 well-studied
- Associated with improved metabolic markers
- May enhance satiety hormone responses
- Found in many probiotic supplements
Lactobacillus Species
Various species affect appetite:
- L. gasseri associated with reduced abdominal fat
- L. rhamnosus may improve satiety
- L. plantarum supports overall gut health
- Different strains have different effects
Signs of Disrupted Appetite Signals
Your appetite regulation may be impaired if you:
- Feel constantly hungry regardless of recent meals
- Never feel truly satisfied after eating
- Experience intense cravings, especially for sugar/carbs
- Can't distinguish between hunger and emotional eating
- Eat past fullness regularly
- Feel hungry again shortly after large meals
- Experience significant hunger swings
- Have lost touch with natural hunger cues
Dietary Strategies for Appetite Balance
Protein at Every Meal
Protein strongly promotes satiety:
- Stimulates GLP-1 and PYY release
- Has high thermic effect
- Helps maintain muscle mass
- Aim for 20-30g per meal
Good sources:
- Eggs and dairy
- Fish and poultry
- Legumes and tofu
- Nuts and seeds
Fiber-Rich Foods
Fiber promotes satiety through multiple mechanisms:
Mechanical fullness:
- Takes up space in the stomach
- Requires more chewing, slowing eating
- Delays gastric emptying
Bacterial fermentation:
- Produces SCFAs that trigger satiety hormones
- Feeds beneficial appetite-regulating bacteria
- Effects build over time with consistent intake
High-satiety fiber sources:
- Legumes (especially effective)
- Oats and barley
- Vegetables
- Whole fruits (not juice)
Fermented Foods
Support appetite-regulating bacteria:
- Provide beneficial species directly
- Support overall microbiome health
- May improve satiety hormone responses
- Include daily for best effects
Mindful Eating Practices
How you eat matters as much as what:
Eat slowly:
- Takes 20 minutes for satiety signals to reach brain
- Chewing thoroughly aids digestion
- Smaller bites naturally slow eating
Minimize distractions:
- Screens during meals reduce satiety
- Paying attention to food enhances satisfaction
- Notice flavors, textures, fullness cues
Use smaller plates:
- Visual cues affect perceived fullness
- Helps align portions with actual needs
- Simple but effective strategy
Foods That Disrupt Appetite
Limit these appetite-dysregulating foods:
Highly processed foods:
- Engineered to override satiety signals
- Combine fat, sugar, and salt in ways that promote overconsumption
- Damage the microbiome
Artificial sweeteners:
- May disrupt appetite signaling
- Some evidence of microbiome effects
- Natural alternatives when sweetness needed
Liquid calories:
- Don't trigger satiety like solid food
- Easy to overconsume
- Includes sodas, juices, many coffees

Lifestyle Factors
Sleep
Sleep deprivation dramatically affects appetite:
- Increases ghrelin (hunger hormone)
- Decreases leptin (fullness hormone)
- Promotes cravings for high-calorie foods
- Even one night of poor sleep affects appetite the next day
Stress
Chronic stress disrupts appetite through:
- Elevated cortisol affecting hunger hormones
- Emotional eating patterns
- Microbiome changes that affect signaling
- Reduced ability to recognize true hunger
Exercise
Physical activity improves appetite regulation:
- Enhances sensitivity to satiety signals
- Improves microbiome diversity
- May reduce hedonic hunger (eating for pleasure vs. need)
- Timing around meals can affect subsequent appetite
Rebuilding Appetite Awareness
Hunger-Fullness Scale
Practice rating hunger on a 1-10 scale:
- 1-2: Extremely hungry, uncomfortable
- 3-4: Hungry, ready to eat
- 5-6: Neutral, comfortable
- 7-8: Satisfied, could stop eating
- 9-10: Overly full, uncomfortable
Aim to eat at 3-4 and stop at 7-8.
Distinguishing Hunger Types
Learn to recognize:
- Physical hunger: Builds gradually, stomach sensations
- Emotional hunger: Sudden, specific cravings, not satisfied by food
- Mouth hunger: Wanting taste without true need
- Habitual hunger: Eating by the clock, not by need
Building Better Appetite Signals
Restoring natural appetite regulation through the microbiome involves:
- Increasing fiber intake to feed SCFA-producing bacteria
- Prioritizing protein for satiety hormone stimulation
- Including fermented foods to support beneficial species
- Practicing mindful eating to reconnect with satiety cues
- Managing sleep and stress for hormonal balance
- Limiting processed foods that override natural signals
Most people notice improved satiety and reduced cravings within 2-4 weeks. Fully restoring natural appetite signals typically takes 2-3 months of consistent practice, but the ability to eat intuitively and maintain healthy weight becomes increasingly natural over time.
Supporting Practices
Evidence-based strategies to support this benefit:
- Eat slowly and mindfully to allow satiety signals to register
- Include protein at every meal for satiety
- Consume high-fiber foods that promote fullness
- Stay hydrated—thirst can masquerade as hunger
- Get adequate sleep to regulate hunger hormones
- Manage stress which disrupts appetite signals
References
- Fetissov SO. Role of the gut microbiota in host appetite control: bacterial growth to animal feeding behaviour. Nature Reviews Endocrinology. 2017;13(1):11-25. doi:10.1038/nrendo.2016.150
- Lucas N, Legrand R, Deroissart C, et al.. Hafnia alvei HA4597 strain reduces food intake and body weight gain and improves body composition, glucose, and lipid metabolism in a mouse model of hyperphagic obesity. Microorganisms. 2019;8(1):35. doi:10.3390/microorganisms8010035
- Breton J, Tennoune N, Lucas N, et al.. Gut commensal E. coli proteins activate host satiety pathways following nutrient-induced bacterial growth. Cell Metabolism. 2016;23(2):324-334. doi:10.1016/j.cmet.2015.10.017
- Alcock J, Maley CC, Aktipis CA. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. BioEssays. 2014;36(10):940-949. doi:10.1002/bies.201400071
- Torres-Fuentes C, Schellekens H, Dinan TG, Cryan JF. The microbiota-gut-brain axis in obesity. The Lancet Gastroenterology & Hepatology. 2017;2(10):747-756. doi:10.1016/S2468-1253(17)30147-4
