Improved Insulin Sensitivity
Enhance your body's ability to respond to insulin and regulate blood sugar through microbiome optimization for better metabolic health.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Insulin Sensitivity Crisis
Insulin resistance—when cells fail to respond properly to insulin's signal—underlies type 2 diabetes, metabolic syndrome, and numerous chronic diseases. It affects an estimated 40% of adults, often silently progressing for years before symptoms appear[3].
While genetics and lifestyle play roles, research has revealed that your gut microbiome is a powerful modulator of insulin sensitivity. This opens new avenues for preventing and addressing metabolic dysfunction through microbiome-focused strategies.
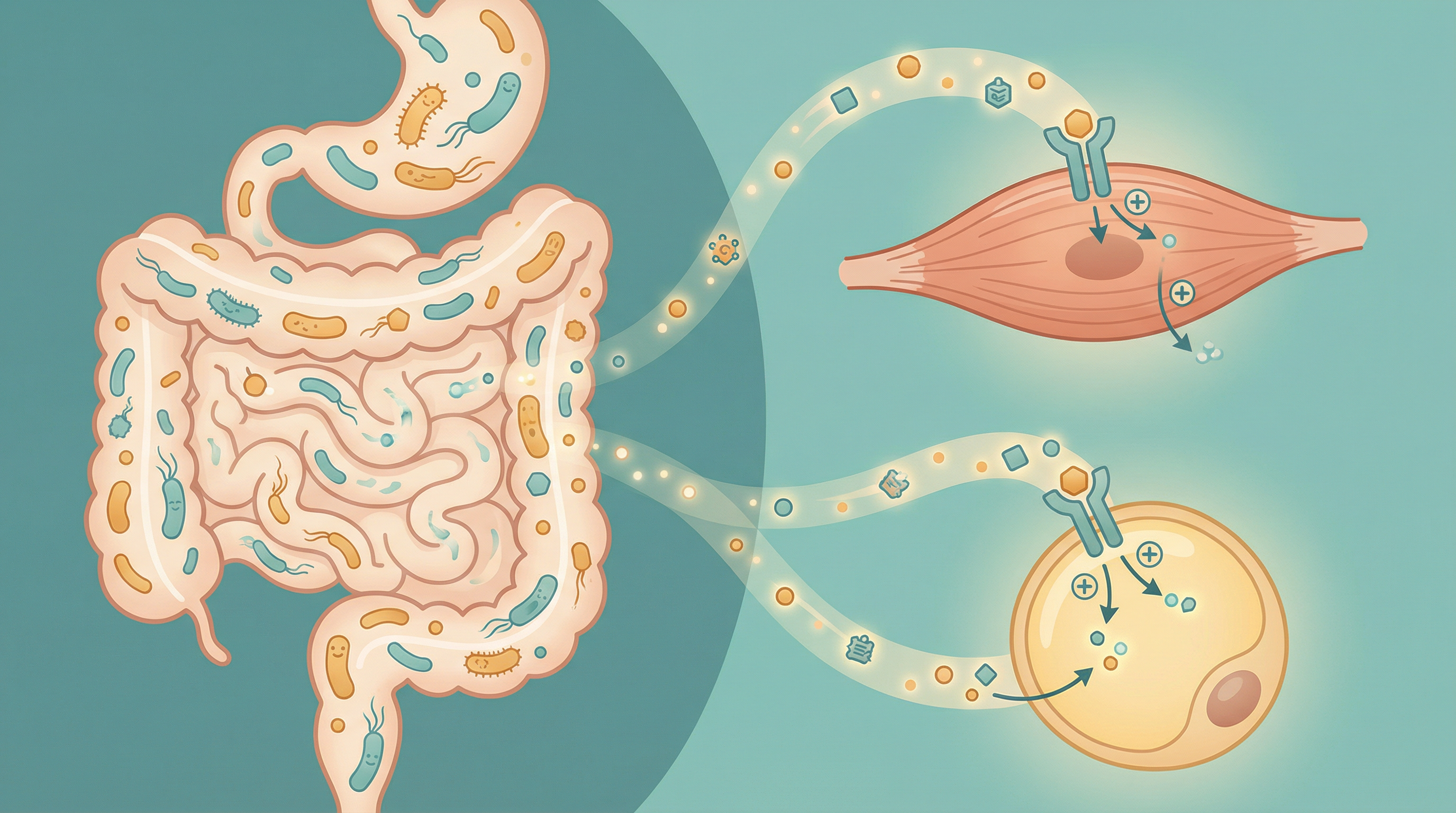
How the Microbiome Affects Insulin Sensitivity
Short-Chain Fatty Acid Production
SCFAs produced by bacterial fermentation of fiber directly improve insulin sensitivity[2]:
Butyrate:
- Activates AMPK (metabolic master switch)
- Improves insulin signaling in muscle and liver
- Reduces inflammation that causes insulin resistance
- Supports healthy gut barrier function
Propionate:
- Stimulates GLP-1 release from gut cells
- GLP-1 enhances insulin secretion and sensitivity
- Reduces hepatic glucose production
- Has satiety-promoting effects
Acetate:
- Influences appetite regulation
- Affects peripheral tissue insulin sensitivity
- Most abundant SCFA
- Important for overall metabolic health
Gut Barrier and Inflammation
A compromised gut barrier contributes to insulin resistance:
- Metabolic endotoxemia: LPS leakage triggers inflammation
- This inflammation directly impairs insulin signaling
- Inflammatory cytokines block insulin receptor function
- Healthy bacteria maintain barrier integrity
Bile Acid Metabolism
Bacterial bile acid modifications affect glucose metabolism:
- Bile acids activate FXR and TGR5 receptors
- These receptors regulate glucose and lipid metabolism
- Bacterial bile salt hydrolase activity shapes bile acid profiles
- Certain bile acid compositions improve insulin sensitivity
Incretin Hormone Regulation
Gut bacteria influence hormones that control insulin:
- GLP-1 enhances insulin secretion and sensitivity
- GIP also affects insulin function
- Bacterial metabolites stimulate incretin release
- This improves glucose handling after meals
Key Metabolic Microbes
Akkermansia muciniphila
Perhaps the most important bacterium for metabolic health[1]:
- Consistently associated with better insulin sensitivity
- Reduced in obesity and type 2 diabetes
- Supplementation improves metabolic markers in humans
- Responds to polyphenol-rich foods
- Research has shown that even a purified membrane protein from A. muciniphila or the pasteurized bacterium improves metabolism[4]
Faecalibacterium prausnitzii
Major butyrate producer with metabolic benefits:
- Abundant in healthy metabolic phenotypes
- Depleted in diabetes and obesity
- Anti-inflammatory effects improve insulin signaling
- Thrives on diverse dietary fiber
Bifidobacterium Species
Foundational for metabolic health:
- Associated with better glucose control
- Support gut barrier function
- Produce acetate and other beneficial metabolites
- Respond well to prebiotic fibers
Roseburia intestinalis
Important butyrate producer:
- Linked to improved insulin sensitivity
- Ferments resistant starch effectively
- Supports healthy glucose metabolism
- Often reduced in metabolic dysfunction
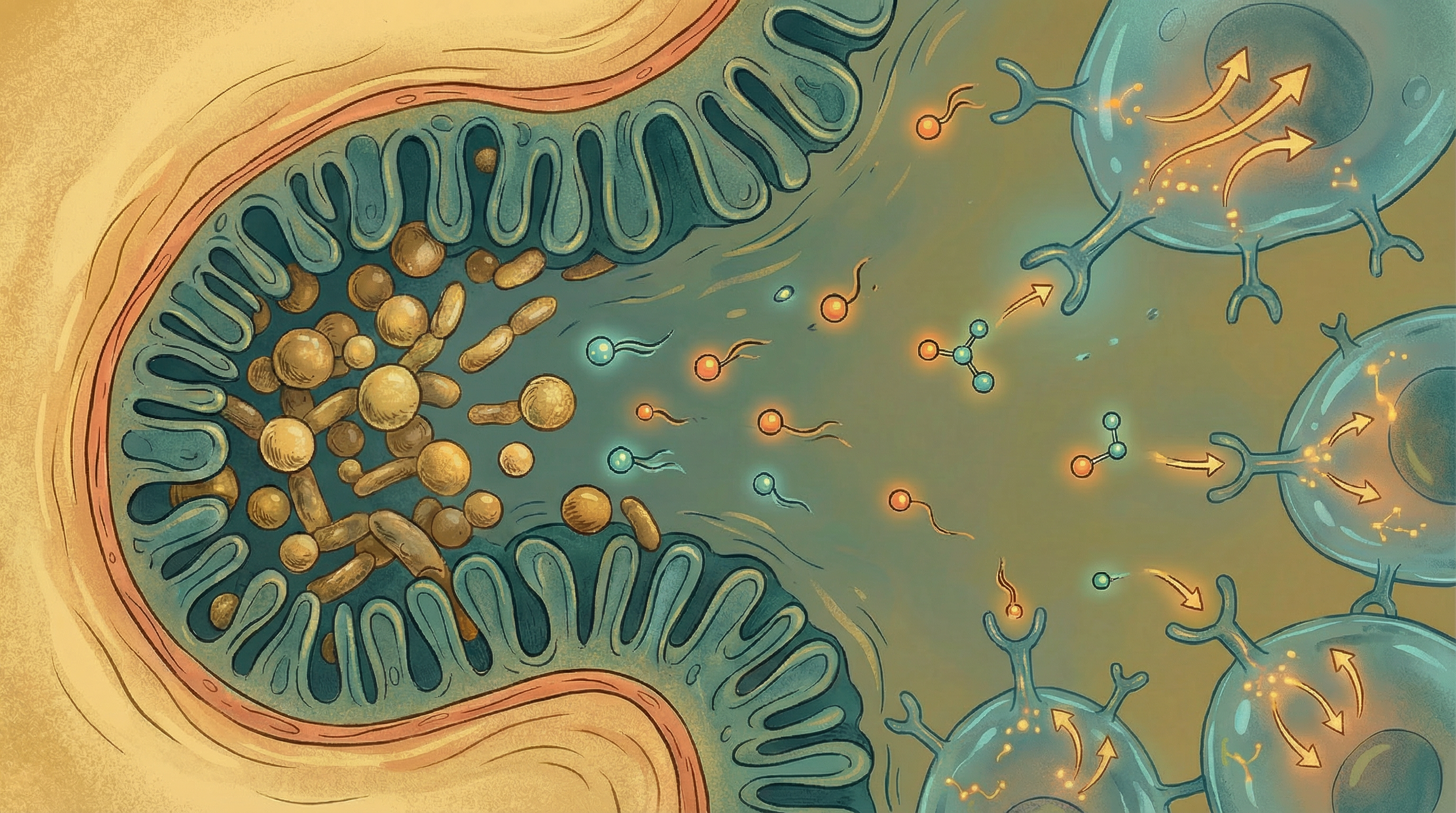
Metagenome-Wide Association Studies
Large-scale genetic studies of the gut microbiome have revealed consistent patterns in type 2 diabetes[6]:
- Patients with T2DM show moderate gut dysbiosis
- Reduced butyrate-producing bacteria
- Increased opportunistic pathogens
- Altered microbial functions related to membrane transport and oxidative stress
European studies have confirmed these findings, showing distinct microbiome signatures across the spectrum from normal to impaired to diabetic glucose control[5].
Signs of Insulin Resistance
Early warning signs include:
- Fatigue, especially after meals
- Sugar and carbohydrate cravings
- Difficulty losing weight, especially around the middle
- Darkened skin patches (acanthosis nigricans)
- Skin tags
- Frequent hunger despite eating
- Brain fog or difficulty concentrating
- High triglycerides, low HDL cholesterol
- Elevated fasting glucose or HbA1c
Dietary Strategies for Insulin Sensitivity
Fiber-First Approach
High-fiber diets dramatically improve insulin sensitivity[2]:
Diverse plant fibers:
- Aim for 30+ different plants weekly
- Include vegetables, fruits, legumes, whole grains
- Vary preparation methods (raw, cooked, fermented)
Resistant starch:
- Cooked and cooled potatoes, rice, and pasta
- Green bananas and plantains
- Legumes
- Supports Akkermansia and butyrate producers
Prebiotic fibers:
- Chicory root and Jerusalem artichokes
- Garlic, onions, and leeks
- Asparagus
- Oats and barley
Polyphenol-Rich Foods
Polyphenols support metabolic bacteria:
- Berries (especially blueberries)
- Green tea and matcha
- Dark chocolate (70%+ cacao)
- Red wine (moderate amounts)
- Pomegranate
- Extra virgin olive oil
Fermented Foods
Support beneficial bacteria:
- Yogurt with live cultures
- Kefir
- Sauerkraut and kimchi
- Miso and tempeh
- Kombucha
Foods to Limit
These impair insulin sensitivity and damage the microbiome:
- Refined sugars and carbohydrates
- Ultra-processed foods
- Artificial sweeteners (some may worsen insulin response)
- Excessive saturated fat
- Alcohol in large amounts

Lifestyle Factors
Exercise
Physical activity powerfully improves insulin sensitivity:
- Both aerobic and resistance training help
- Post-meal walking reduces glucose spikes
- Consistency matters more than intensity
- Exercise also improves microbiome diversity
Meal Timing
When you eat affects insulin sensitivity:
Time-restricted eating:
- Confine eating to 8-12 hour window
- Aligns with circadian rhythms
- Improves metabolic flexibility
- Supports microbiome health
Front-loading calories:
- Eat more earlier in the day
- Insulin sensitivity is highest in the morning
- Lighter evening meals support glucose control
Sleep
Sleep deprivation rapidly impairs insulin sensitivity:
- Just one night of poor sleep affects glucose metabolism
- Chronic sleep debt compounds the problem
- Sleep disruption alters the microbiome
- Aim for 7-9 hours consistently
Stress Management
Chronic stress elevates cortisol, which:
- Directly causes insulin resistance
- Alters the microbiome negatively
- Promotes visceral fat accumulation
- Regular stress management practices help
Testing and Monitoring
Key markers for insulin sensitivity:
- Fasting insulin: Should be below 10 μIU/mL ideally
- HOMA-IR: Calculated from fasting glucose and insulin
- HbA1c: Reflects average glucose over 3 months
- Triglyceride/HDL ratio: Higher ratio indicates resistance
- Oral glucose tolerance test: Shows real-time glucose handling
- Continuous glucose monitor: Reveals individual food responses
Building Better Insulin Sensitivity
Improving insulin sensitivity through the microbiome involves:
- Dramatically increasing fiber intake from diverse sources
- Including polyphenol-rich foods daily
- Adding fermented foods for beneficial bacteria
- Implementing time-restricted eating patterns
- Exercising regularly with emphasis on post-meal activity
- Prioritizing sleep and stress management
Most people notice improvements in energy and reduced cravings within 2-4 weeks. Measurable improvements in insulin sensitivity markers typically develop over 2-3 months of consistent lifestyle changes. Full metabolic restoration may take 6-12 months depending on the starting point.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume fiber-rich foods to feed beneficial bacteria
- Include polyphenol-rich foods like berries and green tea
- Practice time-restricted eating (12-16 hour overnight fast)
- Engage in regular physical activity, especially after meals
- Manage stress which impairs insulin sensitivity
- Prioritize quality sleep for metabolic health
References
- Depommier C, Everard A, Druart C, et al.. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nature Medicine. 2019;25(7):1096-1103. doi:10.1038/s41591-019-0495-2
- Zhao L, Zhang F, Ding X, et al.. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359(6380):1151-1156. doi:10.1126/science.aao5774
- Canfora EE, Meex RCR, Venema K, Blaak EE. Gut microbial metabolites in obesity, NAFLD and T2DM. Nature Reviews Endocrinology. 2019;15(5):261-273. doi:10.1038/s41574-019-0156-z
- Plovier H, Everard A, Druart C, et al.. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nature Medicine. 2017;23(1):107-113. doi:10.1038/nm.4236
- Karlsson FH, Tremaroli V, Nookaew I, et al.. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99-103. doi:10.1038/nature12198
- Qin J, Li Y, Cai Z, et al.. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55-60. doi:10.1038/nature11450
