Optimized Glucose Regulation
Achieve stable blood sugar levels and improved glycemic control through microbiome-supported glucose metabolism.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
Beyond One-Size-Fits-All Nutrition
One of the most surprising discoveries in nutrition science is that the same food can cause dramatically different blood sugar responses in different people. A banana might spike one person's glucose while barely affecting another's. The key difference? Their gut microbiome[1]. This finding has been validated in multiple populations, demonstrating that personalized nutrition based on microbiome features can effectively predict and improve glycemic responses[5].
This revelation has transformed our understanding of glucose regulation from simple calorie counting to a complex interaction between food, microbiome, and individual physiology.
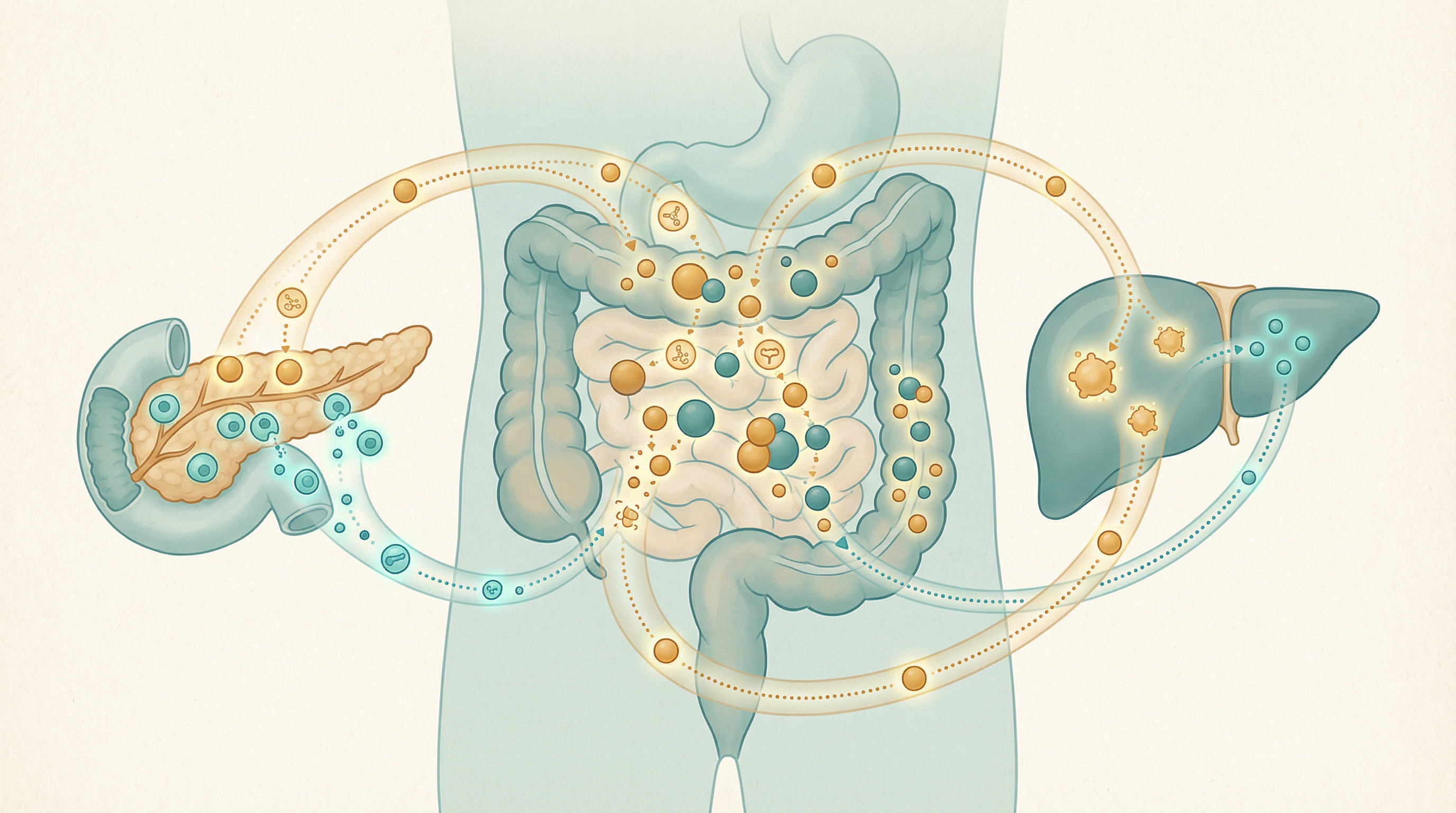
How the Microbiome Regulates Blood Sugar
Incretin Hormone Production
Gut bacteria influence hormones that control glucose[3]:
GLP-1 (Glucagon-like peptide-1):
- Enhances insulin secretion when glucose is high
- Slows gastric emptying, reducing glucose spikes
- Suppresses appetite
- SCFAs from bacterial fermentation stimulate GLP-1 release
GIP (Glucose-dependent insulinotropic peptide):
- Also enhances insulin secretion
- Affected by microbiome composition
- Works synergistically with GLP-1
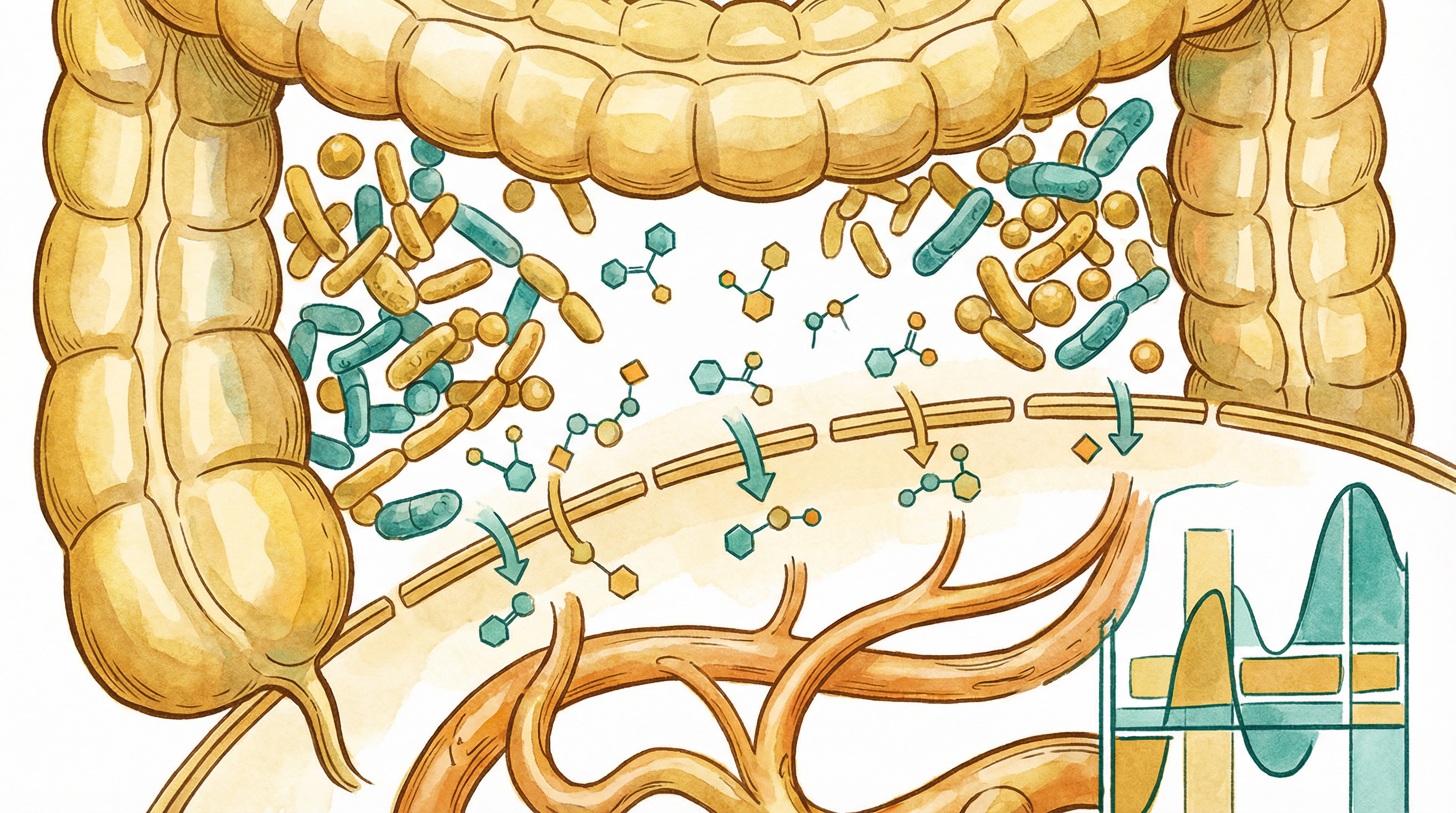
Short-Chain Fatty Acid Effects
SCFAs improve glucose handling through multiple mechanisms[4]:
- Stimulate incretin hormone release
- Improve insulin sensitivity in tissues
- Reduce hepatic glucose production
- Provide alternative fuel that spares glucose
Bile Acid Signaling
Bacterial bile acid modifications affect glucose:
- Activate FXR, which regulates glucose metabolism
- Activate TGR5, which stimulates GLP-1 release
- Affect how glucose is handled by the liver
- Influence overall metabolic flexibility
Inflammation and Glucose
Gut-driven inflammation impairs glucose control:
- Inflammatory cytokines cause insulin resistance
- LPS from leaky gut worsens glucose tolerance
- Anti-inflammatory bacteria improve glycemic control
- Barrier integrity is essential for glucose regulation
Personalized Glycemic Responses
The Microbiome Connection
Research shows microbiome composition predicts individual glycemic responses[1]:
- People with similar microbiomes respond similarly to foods
- Microbiome features predict glucose spikes better than food composition
- This explains why generic diet advice fails many people
- Personalized approaches based on microbiome show superior results
Factors That Vary Responses
Beyond microbiome, responses depend on:
- Recent meals and overall dietary pattern
- Sleep quality the night before
- Stress levels
- Exercise timing
- Time of day (circadian effects)
- Individual genetics
Key Microbes for Glucose Regulation
Prevotella copri
Complex relationship with glucose[2]:
- Associated with improved glucose tolerance in some contexts
- Particularly beneficial when consuming high-fiber foods
- May worsen glucose in low-fiber, high-fat diets
- Context and diet matter significantly
Bifidobacterium adolescentis
Supports healthy glucose metabolism:
- Produces SCFAs that stimulate incretin release
- Associated with better postprandial glucose control
- Thrives on diverse dietary fiber
- Common in metabolically healthy individuals
Akkermansia muciniphila
Metabolic keystone species:
- Consistently linked to better glucose control
- Improves barrier function, reducing inflammation
- Responds to polyphenols and fiber
- Being developed as a therapeutic probiotic
Eubacterium rectale
Major butyrate producer:
- Supports insulin sensitivity
- Ferments resistant starch effectively
- Often depleted in type 2 diabetes
- Responds well to prebiotic foods
Signs of Poor Glucose Regulation
Watch for these indicators:
- Energy crashes, especially after meals
- Intense sugar cravings
- Difficulty concentrating (brain fog)
- Irritability when hungry ("hangry")
- Excessive thirst or frequent urination
- Slow wound healing
- Frequent infections
- Weight gain, especially abdominal
Dietary Strategies for Glucose Control
Food Order Matters
Simple changes in eating order reduce glucose spikes:
- Vegetables/fiber first — creates a gel that slows absorption
- Protein and fat second — further slows gastric emptying
- Carbohydrates last — absorbed more gradually
This can reduce glucose spikes by 30-40% without changing what you eat.
Fiber with Every Meal
Fiber consistently improves glucose responses:
Soluble fiber:
- Oats and barley
- Legumes
- Apples and citrus
- Psyllium husk
Insoluble fiber:
- Vegetables
- Whole grains
- Nuts and seeds
Resistant starch:
- Cooked and cooled potatoes/rice
- Green bananas
- Legumes
Vinegar and Acidic Foods
Acetic acid blunts glucose responses:
- Apple cider vinegar (1-2 tbsp before meals)
- Fermented foods
- Lemon juice
- Mechanism involves delayed gastric emptying and improved insulin sensitivity
Blood Sugar-Stabilizing Foods
Include regularly:
- Cinnamon (may improve insulin sensitivity)
- Fenugreek
- Bitter melon
- Berberine-containing herbs
- Chromium-rich foods (broccoli, eggs)
Foods to Approach Mindfully
These cause larger glucose responses:
- Refined carbohydrates and white flour products
- Sugary drinks (including fruit juices)
- White rice and potatoes (unless cooled)
- Low-fiber breakfast cereals
- Most processed snack foods

Meal Timing and Glucose
Time-Restricted Eating
Eating within consistent windows improves glucose:
- 8-12 hour eating windows show benefits
- Aligns eating with circadian insulin sensitivity
- Morning meals are typically handled better
- Evening carbohydrates may spike more
Post-Meal Movement
Walking after meals significantly reduces glucose spikes:
- Even 10-15 minutes helps
- Works by increasing glucose uptake into muscles
- Most effective started within 30 minutes of eating
- Light activity is sufficient
Meal Frequency
Evidence is mixed, but consider:
- Fewer, larger meals may be better than constant grazing
- Allows insulin to return to baseline between meals
- May support metabolic flexibility
- Individual responses vary
Lifestyle Factors
Sleep
Poor sleep dramatically worsens glucose control:
- One night of poor sleep reduces insulin sensitivity
- Disrupts hormones that regulate appetite and glucose
- Affects microbiome composition
- Prioritize consistent, quality sleep
Stress
Chronic stress elevates cortisol, which:
- Raises blood glucose directly
- Causes insulin resistance
- Promotes comfort eating of high-sugar foods
- Alters microbiome unfavorably
Exercise
Physical activity improves glucose handling:
- Acute effects: muscles take up glucose during exercise
- Chronic effects: improved insulin sensitivity lasting 24-72 hours
- Both aerobic and resistance training beneficial
- Consistency matters most
Monitoring Your Glucose
Consider these approaches:
- Continuous glucose monitor: Real-time feedback on food responses
- Fasting glucose: Morning measurement
- HbA1c: Average glucose over 3 months
- Oral glucose tolerance test: How you handle a glucose load
- Food-glucose diary: Track patterns in your responses
Building Better Glucose Control
Optimizing glucose regulation through the microbiome involves:
- Prioritizing fiber with every meal
- Strategic food ordering (vegetables → protein → carbs)
- Post-meal movement to enhance glucose uptake
- Time-restricted eating aligned with circadian rhythms
- Supporting beneficial bacteria through prebiotic and fermented foods
- Managing stress and sleep for hormonal balance
Most people notice improved energy and reduced cravings within 2-4 weeks. Measurable improvements in glucose markers typically develop over 2-3 months of consistent practice. Establishing truly optimized glucose metabolism is an ongoing process that improves steadily with sustained effort.
Supporting Practices
Evidence-based strategies to support this benefit:
- Eat fiber before carbohydrates to blunt glucose spikes
- Take a short walk after meals
- Include vinegar with meals (apple cider vinegar)
- Consume cinnamon regularly
- Practice mindful, slower eating
- Stay well-hydrated throughout the day
References
- Zeevi D, Korem T, Zmora N, et al.. Personalized Nutrition by Prediction of Glycemic Responses. Cell. 2015;163(5):1079-1094. doi:10.1016/j.cell.2015.11.001
- Kovatcheva-Datchary P, Nilsson A, Akrami R, et al.. Dietary Fiber-Induced Improvement in Glucose Metabolism Is Associated with Increased Abundance of Prevotella. Cell Metabolism. 2015;22(6):971-982. doi:10.1016/j.cmet.2015.10.001
- Tolhurst G, Heffron H, Lam YS, et al.. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes. 2012;61(2):364-371. doi:10.2337/db11-1019
- Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell. 2016;165(6):1332-1345. doi:10.1016/j.cell.2016.05.041
- Mendes-Soares H, Raveh-Sadka T, Azulay S, et al.. Assessment of a personalized approach to predicting postprandial glycemic responses to food among individuals without diabetes. JAMA Network Open. 2019;2(2):e188102. doi:10.1001/jamanetworkopen.2018.8102
