Reduced Skin Inflammation
Calm inflammatory skin conditions and reduce redness through gut microbiome optimization for clearer, more comfortable skin.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
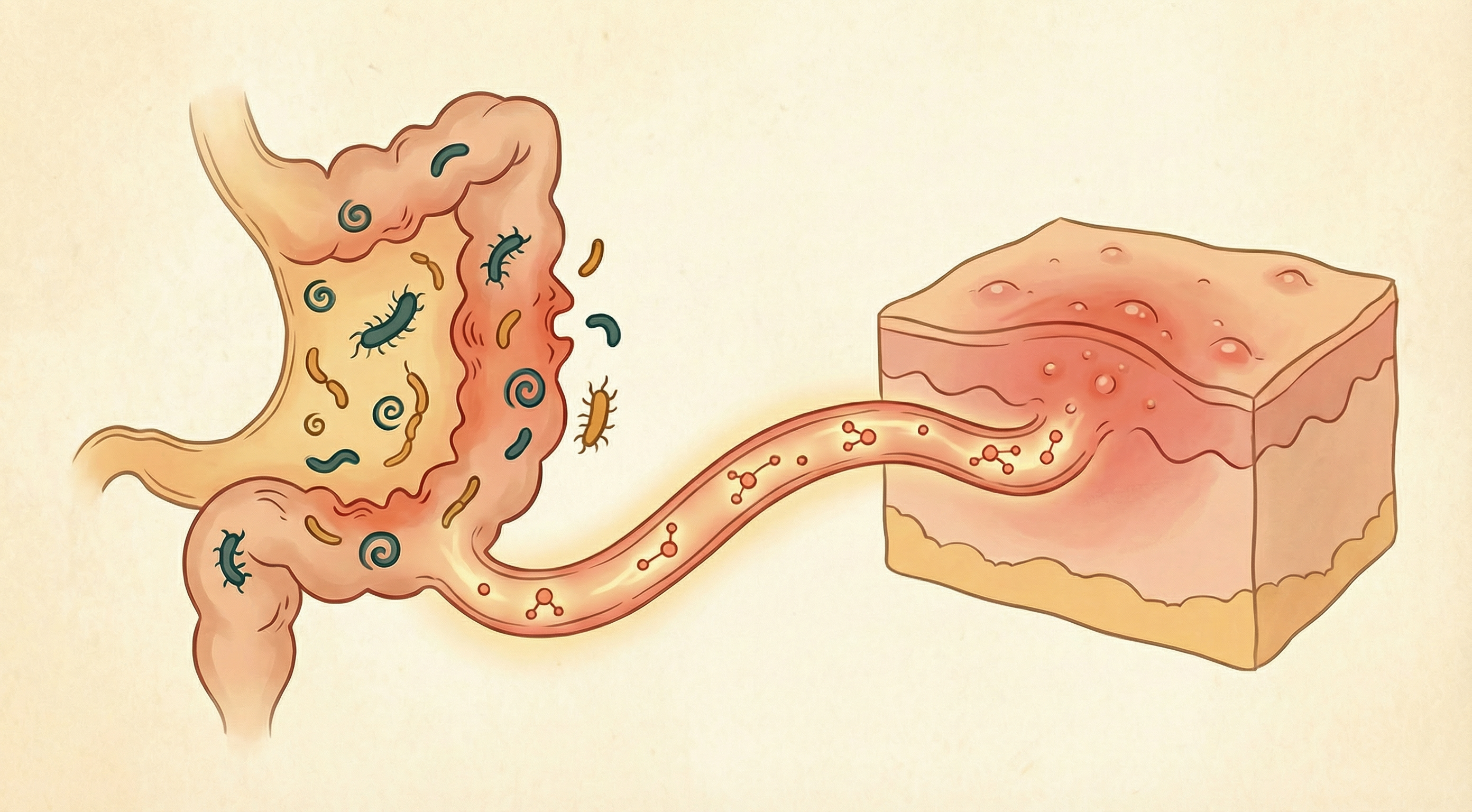
The Inflammation-Skin Connection
Many common skin conditions—acne, eczema, psoriasis, rosacea—share a common underlying feature: inflammation. While topical treatments address surface symptoms, research increasingly shows that skin inflammation often originates in or is exacerbated by the gut.[1]
The gut-brain-skin axis explains why stress, diet, and gut health all affect inflammatory skin conditions. Addressing gut health can provide relief that topical treatments alone cannot achieve.
How Gut Dysbiosis Drives Skin Inflammation
Systemic Inflammatory Signaling
When the gut is inflamed, the whole body feels it:
- Inflammatory cytokines (IL-1, IL-6, TNF-α) enter circulation
- These reach the skin and activate inflammatory pathways
- Immune cells in skin respond by mounting inflammatory responses
- This manifests as redness, swelling, pustules, or plaques
Increased Intestinal Permeability
"Leaky gut" contributes to skin inflammation:
- LPS and other bacterial products enter bloodstream
- These trigger systemic immune activation
- The skin, as a highly vascular organ, is affected
- Barrier dysfunction in gut often parallels barrier dysfunction in skin
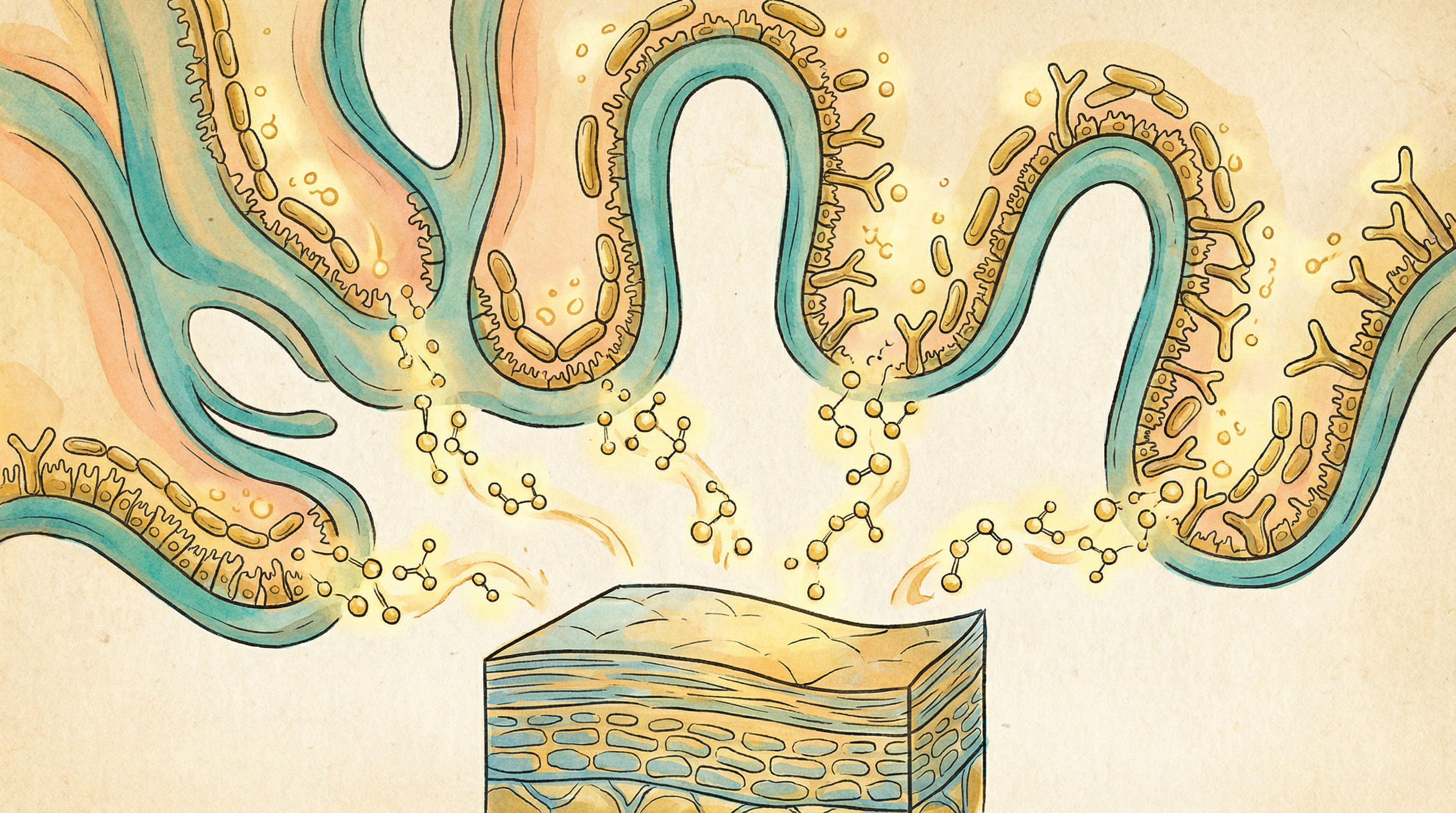
Altered Immune Regulation
Gut bacteria shape immune responses that affect skin:
- Determine balance between tolerance and reactivity
- Influence Th1/Th2/Th17 immune balance
- Affect regulatory T cell function
- Dysbiosis can skew toward inflammatory responses
Nutrient Deficiencies
Gut problems can cause deficiencies that promote skin inflammation:
- Zinc deficiency common in inflammatory skin conditions
- Essential fatty acid malabsorption
- Vitamin A and D status affected by gut health
- All these nutrients are crucial for calming skin inflammation
Skin Conditions Linked to Gut Dysbiosis
Acne
The gut-acne connection is well-established:[2]
- Acne patients often have different gut bacteria than controls
- SIBO (small intestinal bacterial overgrowth) more common in acne
- High-glycemic diets worsen both gut and acne
- Probiotics have shown benefit in clinical trials
Eczema (Atopic Dermatitis)
Strong gut-skin connection in eczema:
- Often begins with gut issues in infancy
- Food sensitivities frequently involved
- Gut permeability increased in many patients
- Early probiotic use may prevent eczema development
Psoriasis
Autoimmune condition with gut involvement:[3]
- Distinct gut microbiome patterns in psoriasis
- Metabolic syndrome often co-occurs
- Dietary interventions can improve symptoms
- Gut inflammation precedes flares in some patients
Rosacea
Gut connection increasingly recognized:
- SIBO significantly more common in rosacea
- H. pylori infection may be involved
- Treating gut often improves facial symptoms
- Certain foods trigger both gut and skin symptoms
Key Anti-Inflammatory Microbes
Lactobacillus rhamnosus
Most studied for skin inflammation:
- Reduces inflammatory markers
- Improves skin barrier function
- Strain GG prevents eczema in high-risk infants
- Benefits both gut and skin inflammation
Bifidobacterium lactis
Supports anti-inflammatory pathways:
- Reduces systemic inflammation markers
- Improves gut barrier integrity
- Associated with better skin outcomes
- Well-tolerated in clinical studies
Faecalibacterium prausnitzii
Potent anti-inflammatory effects:
- Major butyrate producer
- Secretes anti-inflammatory proteins
- Often depleted in inflammatory conditions
- Responds to dietary fiber
Lactobacillus acidophilus
Foundational probiotic for skin:
- Reduces skin sensitivity and reactivity
- Supports healthy immune responses
- Part of many effective probiotic combinations
- Long safety track record
Dietary Strategies to Reduce Skin Inflammation
Anti-Inflammatory Foods
Omega-3 fatty acids:
- Fatty fish (salmon, sardines, mackerel)
- Walnuts and flaxseeds
- Compete with pro-inflammatory omega-6s
- Direct anti-inflammatory effects on skin
Polyphenol-rich foods:
- Green tea (EGCG is particularly anti-inflammatory)
- Berries (especially blueberries)
- Turmeric (with black pepper for absorption)
- Dark chocolate
Fermented foods:
- Introduce anti-inflammatory bacteria
- Support overall gut health
- Daily consumption recommended
Fiber-rich foods:
- Feed butyrate-producing bacteria
- Support gut barrier function
- Reduce systemic inflammation
Inflammatory Triggers to Limit
High-glycemic foods:
- Spike insulin, which increases inflammation
- Directly worsen acne
- Include white bread, sugary foods, white rice
- Choose whole grain, low-glycemic alternatives
Dairy (for some people):
- May trigger inflammation in sensitive individuals
- Hormones in milk may affect skin
- A1 casein particularly problematic for some
- Trial elimination to assess personal response
Common food allergens:
- Gluten affects some with skin conditions
- Eggs, soy, nuts can be triggers
- Elimination and reintroduction helps identify
- Work with healthcare provider for guidance
Alcohol:
- Directly inflammatory
- Triggers rosacea flares
- Disrupts gut microbiome
- Dehydrates skin
Elimination Approach
To identify personal triggers:
- Remove common triggers for 3-4 weeks
- Monitor skin carefully
- Reintroduce one food at a time
- Watch for reactions over 3-4 days
- Keep a food-skin diary

Lifestyle Factors
Stress Management
Stress directly triggers skin inflammation:
- Increases cortisol and inflammatory cytokines
- Activates mast cells in skin
- Disrupts gut barrier function
- Links brain, gut, and skin in inflammation cascade
Helpful practices:
- Regular meditation or mindfulness
- Deep breathing exercises
- Yoga or gentle movement
- Adequate rest and boundaries
Sleep
Poor sleep worsens inflammation:
- Increases inflammatory markers
- Impairs skin repair
- Worsens stress response
- Disrupts gut-skin axis
Prioritize 7-9 hours of quality sleep.
Exercise
Moderate exercise reduces inflammation:
- Lowers inflammatory markers over time
- Improves gut microbiome diversity
- Reduces stress
- Avoid over-exercising, which can increase inflammation
Environmental Factors
Consider external triggers:
- Harsh skincare products
- Pollution exposure
- Extreme temperatures
- Synthetic fabrics against skin
Targeted Probiotic Approach
For specific conditions, research supports:
Acne:
- Lactobacillus rhamnosus
- Lactobacillus acidophilus
- Bifidobacterium bifidum
Eczema:
- Lactobacillus rhamnosus GG
- Lactobacillus reuteri
- Bifidobacterium lactis
Rosacea:
- Address underlying gut issues first
- SIBO treatment if present
- General gut-supporting probiotics
Building Calmer Skin
Reducing skin inflammation through the gut involves:
- Identifying and removing personal inflammatory triggers
- Supporting anti-inflammatory bacteria through diet
- Including omega-3s and polyphenols daily
- Managing stress which amplifies inflammation
- Healing gut permeability to reduce systemic inflammation
- Being patient — skin inflammation takes time to calm
Most people notice reduced redness and fewer breakouts within 4-6 weeks of consistent gut-supporting practices. Chronic inflammatory conditions may take 3-6 months to show significant improvement, but addressing root causes provides more lasting relief than topical treatments alone.
Supporting Practices
Evidence-based strategies to support this benefit:
- Eliminate or reduce common inflammatory triggers (dairy, gluten for some)
- Include anti-inflammatory omega-3 fatty acids
- Consume polyphenol-rich foods like green tea and berries
- Avoid high-glycemic foods that spike insulin and inflammation
- Manage stress which exacerbates skin inflammation
- Identify personal food triggers through elimination protocols
References
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future?. Gut Pathogens. 2011;3(1):1. doi:10.1186/1757-4749-3-1 ↩
- Lee YB, Byun EJ, Kim HS. Potential role of the microbiome in acne: A comprehensive review. Journal of Clinical Medicine. 2019;8(7):987. doi:10.3390/jcm8070987 ↩
- Drago L, De Grandi R, Altomare G, et al.. Skin microbiota of first cousins affected by psoriasis and atopic dermatitis. Clinical and Molecular Allergy. 2016;14:2. doi:10.1186/s12948-016-0038-z ↩