Mycoplasma pneumoniae
Key Characteristics
Mycoplasma pneumoniae is a unique and specialized bacterium with several distinctive features that set it apart from conventional bacteria:
- One of the smallest self-replicating organisms capable of cell-free existence
- Lacks a cell wall (belongs to class Mollicutes), making it naturally resistant to beta-lactam antibiotics
- Extremely small genome size (816 kb) with limited metabolic capabilities
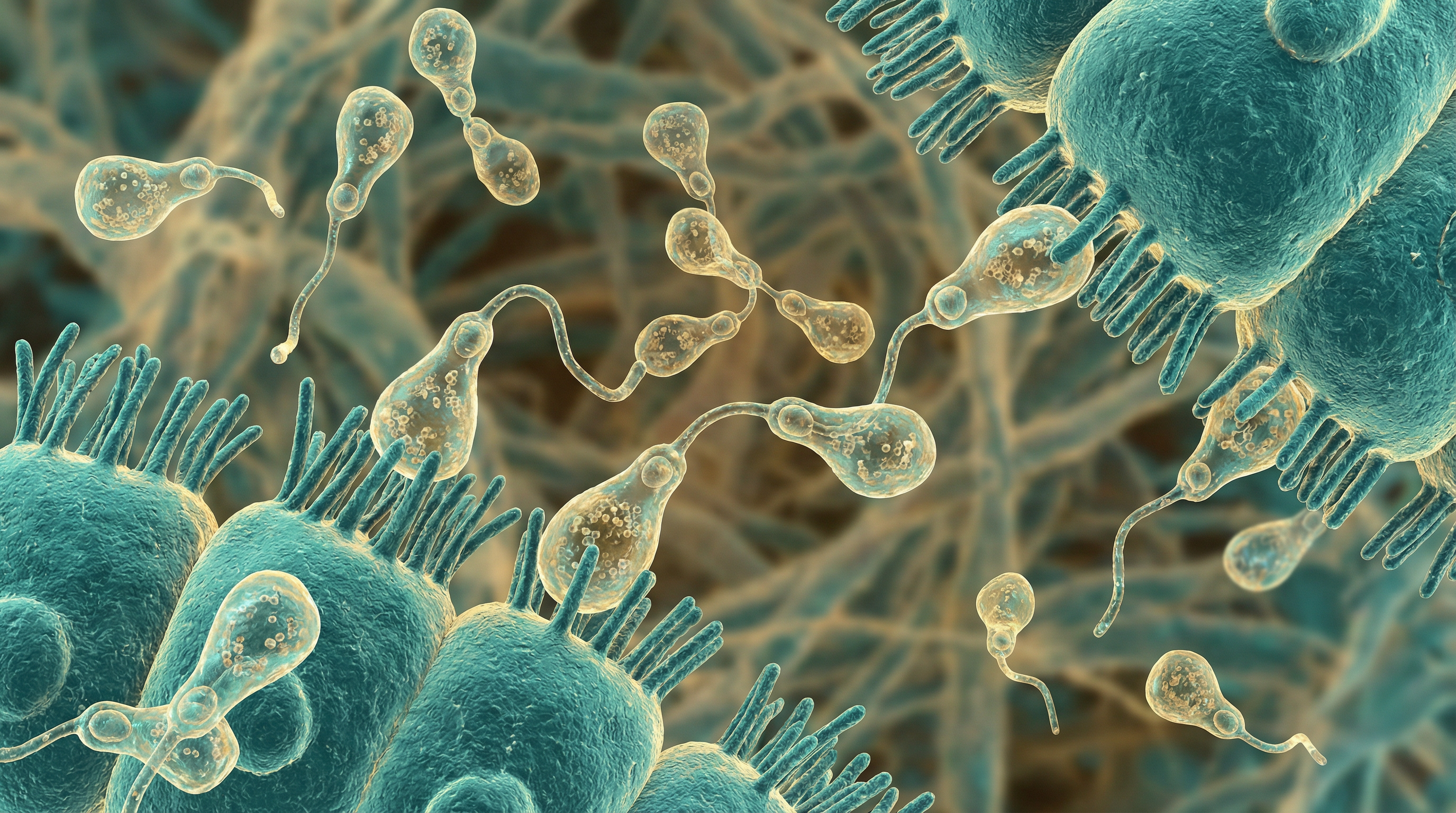
- Pleomorphic in shape, typically appearing as filamentous or flask-shaped cells
- Size ranges from 0.2 to 0.8 μm, requiring specialized microscopy for visualization
- Obligate parasite of humans with no known environmental reservoir
- Requires close host association for survival due to limited biosynthetic capabilities
- Possesses a specialized terminal organelle (attachment organelle) for host cell adhesion
- Slow-growing with generation times of 6 hours or more under optimal conditions
- Requires complex media containing sterols for laboratory cultivation
- Fastidious growth requirements, making laboratory culture challenging
- Primarily aerobic metabolism but can survive in microaerophilic conditions
- Possesses a unique gliding motility mechanism without flagella
- Exhibits cytadherence as a primary virulence mechanism
- Produces hydrogen peroxide and superoxide radicals as virulence factors
- Contains unique membrane lipoproteins that interact with host immune system
- Possesses CARDS (Community-Acquired Respiratory Distress Syndrome) toxin
- Capable of intracellular invasion and persistence within host cells
- Exhibits antigenic variation through DNA recombination
- Possesses mechanisms to evade host immune responses
- Transmits primarily through respiratory droplets from person to person
- Causes both endemic and epidemic respiratory disease patterns
- Exhibits a unique epidemiological pattern with 4-7 year cycles of increased incidence
- Demonstrates seasonal variation with peaks in late summer to early fall
- Affects all age groups but particularly common in school-aged children and young adults
- Incubation period of 1-4 weeks before symptom onset
- Capable of causing prolonged carrier states in some individuals
- Exhibits extrapulmonary spread to multiple organ systems
- Possesses unique surface adhesins (P1 adhesin) essential for pathogenicity
- Demonstrates limited genetic diversity compared to other bacterial pathogens
Mycoplasma pneumoniae represents a highly specialized bacterial pathogen that has evolved a minimalist approach to survival, shedding unnecessary genetic material while retaining essential pathogenic mechanisms. Its unique biological characteristics contribute to its success as a human pathogen and present challenges for diagnosis, treatment, and control.
Role in Human Microbiome
Mycoplasma pneumoniae occupies a specialized niche within the human microbiome, primarily associated with the respiratory tract:
Respiratory Tract Colonization:
- Primarily colonizes the ciliated epithelium of the respiratory tract
- Can be found in both upper and lower respiratory tract
- Attaches to respiratory epithelial cells via specialized adhesins
- Not considered part of the normal respiratory microbiota
- Typically present as a pathogen rather than a commensal organism
- Colonization rates increase during epidemic periods
- Can persist in the respiratory tract for weeks to months after infection
- Asymptomatic carriage occurs, particularly in children
- Carrier state may serve as a reservoir for transmission
- Colonization patterns influenced by age, with higher rates in school-aged children
Interactions with Respiratory Microbiome:
- Disrupts the normal respiratory microbiome during infection
- Reduces overall microbial diversity in the respiratory tract
- Alters the balance of commensal bacteria during infection
- May create conditions favorable for secondary bacterial infections
- Interacts with other respiratory pathogens in co-infections
- Synergistic relationships with some viral respiratory pathogens
- Competition with normal respiratory flora for nutrients and attachment sites
- Influences host immune responses to other microbiome members
- Alters respiratory epithelial cell function, affecting microbial balance
- Recovery of normal microbiome composition may take weeks after infection
Transmission and Spread:
- Transmitted primarily through respiratory droplets
- Person-to-person spread through close contact
- Prolonged close contact increases transmission risk
- Household and classroom settings are common transmission sites
- Incubation period of 1-4 weeks before symptom onset
- Can be shed from respiratory tract for several weeks after infection
- Asymptomatic carriers can transmit the organism
- Outbreaks common in closed or semi-closed communities
- Transmission facilitated by crowded living conditions
- No known environmental reservoir or vector
Population Dynamics:
- Affects all age groups but particularly common in school-aged children
- Exhibits cyclic epidemic patterns every 4-7 years
- Seasonal variation with peaks in late summer to early fall
- Endemic transmission occurs between epidemic periods
- Immunity after infection is incomplete and temporary
- Reinfections can occur throughout life
- Population immunity influences epidemic cycles
- Geographic variations in prevalence and strain distribution
- Urban populations typically have higher prevalence than rural
- School attendance strongly associated with transmission patterns
Ecological Adaptations:
- Highly adapted to the human respiratory epithelium
- Specialized attachment mechanisms for human cell receptors
- Limited metabolic capabilities compensated by host resource utilization
- Evolved mechanisms to evade host immune responses
- Adapted to survive in different regions of the respiratory tract
- Capable of intracellular invasion for protection from host defenses
- Biofilm formation capabilities in some conditions
- Persistence mechanisms for long-term colonization
- Antigenic variation to evade host adaptive immunity
- Minimal genome optimized for parasitic lifestyle
Microbiome Disruption During Disease:
- Significant increase in relative abundance during active infection
- Displacement of normal commensal bacteria
- Reduction in overall microbiome diversity
- Altered functional capacity of the respiratory microbiome
- Inflammatory response affects other microbiome members
- Disruption of normal microbiome-host interactions
- Changes in local microenvironment affecting microbial growth
- Altered nutrient availability for other microbiome members
- Potential for long-term microbiome alterations after infection
- Possible role in post-infectious dysbiosis
Unlike many other bacteria covered in this collection, Mycoplasma pneumoniae is not considered a normal component of the healthy human microbiome. Instead, it represents a specialized respiratory pathogen that temporarily colonizes and disrupts the respiratory microbiome during infection. Its unique biological characteristics and host adaptations allow it to successfully establish infection and transmission within human populations, making it a significant cause of respiratory disease worldwide.
Health Implications
Mycoplasma pneumoniae infections have significant health implications, ranging from mild respiratory symptoms to severe complications:
Respiratory Manifestations:
Tracheobronchitis (Chest Cold): Most common presentation with gradual onset
- Persistent, slowly worsening cough that may last for weeks
- Low-grade fever, fatigue, and headache
- Sore throat and occasional hoarseness
- Generally self-limiting but prolonged course
"Walking Pneumonia": Atypical pneumonia with milder symptoms than typical bacterial pneumonia
- Patients often ambulatory despite lung infection
- Dry, non-productive cough that may become productive later
- Fever, chills, and malaise
- Chest pain or discomfort
- Shortness of breath, especially with exertion
- Radiographic findings often more severe than clinical presentation suggests
Severe Pneumonia: Less common but significant, especially in vulnerable populations
- High fever and significant respiratory distress
- May require hospitalization and oxygen support
- More common in immunocompromised individuals
- Can progress to respiratory failure in severe cases
- Pleural effusions may develop
Upper Respiratory Tract Infections:
- Pharyngitis (sore throat)
- Rhinitis (nasal inflammation)
- Sinusitis
- Otitis media (middle ear infection)
- Bullous myringitis (painful ear blisters)
Extrapulmonary Complications:
Dermatological Manifestations:
- Stevens-Johnson syndrome (severe mucocutaneous reaction)
- Mycoplasma-induced rash and mucositis (MIRM)
- Erythema multiforme
- Urticaria and other rashes
Neurological Complications:
- Encephalitis (brain inflammation)
- Meningitis (meningeal inflammation)
- Guillain-Barré syndrome (ascending paralysis)
- Transverse myelitis
- Acute disseminated encephalomyelitis (ADEM)
- Peripheral neuropathies
- Cerebellar ataxia
- Stroke-like syndromes
Hematological Manifestations:
- Hemolytic anemia (destruction of red blood cells)
- Thrombocytopenia (low platelet count)
- Disseminated intravascular coagulation (rare)
- Thrombotic events
Cardiovascular Complications:
- Myocarditis (heart muscle inflammation)
- Pericarditis (pericardium inflammation)
- Cardiac arrhythmias
Gastrointestinal Manifestations:
- Hepatitis
- Pancreatitis
- Gastroenteritis-like symptoms
Musculoskeletal Complications:
- Arthritis and arthralgia
- Myositis (muscle inflammation)
- Rhabdomyolysis (rare)
Renal Complications:
- Glomerulonephritis
- Tubulointerstitial nephritis
- Renal dysfunction
Special Population Considerations:
Children:
- Higher incidence of infection
- May present with different symptoms (diarrhea, vomiting, wheezing)
- More likely to develop extrapulmonary complications
- Important cause of community-acquired pneumonia in school-aged children
- May trigger new-onset asthma or exacerbate existing asthma
Elderly:
- More severe disease course
- Higher risk of hospitalization
- Increased mortality compared to younger adults
- Often misdiagnosed due to atypical presentation
- Comorbidities complicate management
Immunocompromised Individuals:
- More severe and prolonged infections
- Higher risk of extrapulmonary spread
- May develop chronic infection
- Reduced response to antibiotic therapy
- Higher mortality rates
Patients with Underlying Respiratory Conditions:
- Exacerbation of asthma and COPD
- More severe disease course
- Prolonged recovery period
- Higher risk of respiratory failure
- May require more aggressive treatment
Long-term Health Impacts:
Chronic Respiratory Symptoms:
- Persistent cough for weeks to months
- Reduced lung function in some patients
- Bronchial hyperreactivity
- Possible role in chronic asthma pathogenesis
Post-infectious Fatigue Syndrome:
- Prolonged fatigue and malaise
- Reduced exercise tolerance
- Cognitive difficulties
- Similar to chronic fatigue syndrome in some cases
Recurrent Infections:
- Incomplete immunity after infection
- Possibility of reinfection
- Potential for chronic carriage in some individuals
Psychological Impact:
- Anxiety related to prolonged symptoms
- Depression associated with chronic illness
- Impact on quality of life and daily activities
- School or work absenteeism
Public Health Implications:
Epidemic Potential:
- Cyclic outbreaks every 4-7 years
- Significant burden on healthcare systems during epidemics
- Outbreaks in closed communities (schools, military bases, etc.)
Antibiotic Resistance:
- Increasing macrolide resistance globally
- Treatment challenges in areas with high resistance
- Need for antibiotic stewardship
Diagnostic Challenges:
- Often misdiagnosed as viral infection
- Limited availability of rapid diagnostic tests
- Underreporting of actual disease burden
Economic Impact:
- Healthcare costs for diagnosis and treatment
- Lost productivity due to prolonged illness
- School and work absenteeism
- Costs associated with managing complications
The health implications of Mycoplasma pneumoniae infections are broad and significant, ranging from mild respiratory symptoms to severe, life-threatening complications. The organism's ability to cause extrapulmonary manifestations and its impact on special populations make it an important pathogen from both clinical and public health perspectives. The prolonged nature of symptoms and potential for long-term health effects further underscore its significance as a human pathogen.
Metabolic Activities
Mycoplasma pneumoniae exhibits unique metabolic activities that reflect its highly adapted parasitic lifestyle and minimal genome:
Energy Metabolism:
- Primarily relies on glycolysis for ATP generation
- Lacks a complete tricarboxylic acid (TCA) cycle
- Absence of oxidative phosphorylation and electron transport chain
- Generates ATP through substrate-level phosphorylation
- Utilizes the pentose phosphate pathway for NADPH production
- Lacks most anabolic pathways, requiring host-derived nutrients
- Produces lactic acid as a major fermentation end product
- Limited capacity for alternative energy sources beyond glucose
- Possesses specialized transporters for nutrient acquisition from host
- Energy metabolism optimized for minimal genome size
Carbohydrate Metabolism:
- Glucose is the primary carbon and energy source
- Possesses complete glycolytic pathway enzymes
- Limited capacity for metabolism of other sugars
- Lacks enzymes for gluconeogenesis
- Unable to s (Content truncated due to size limit. Use line ranges to read in chunks)
