Acne
Explore the connection between gut microbiome imbalances and acne, and discover evidence-based approaches for managing skin health through microbiome optimization.
Common Symptoms
Microbiome Imbalances
Research has identified the following microbiome patterns commonly associated with this condition:
- Gut dysbiosis
- Increased intestinal permeability
- Elevated Cutibacterium acnes
- Reduced skin microbiome diversity
Understanding Acne and the Microbiome Connection
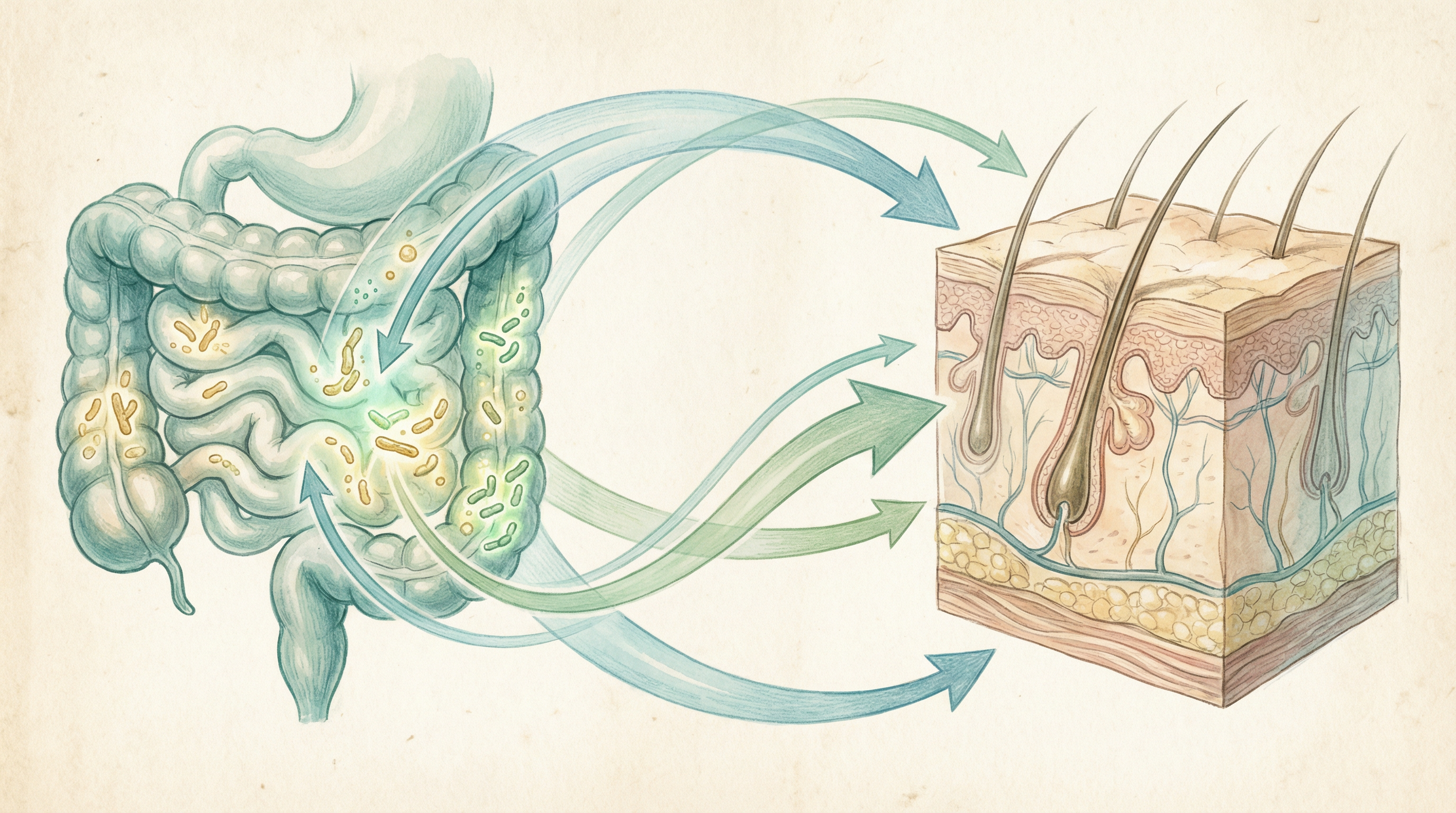
Acne vulgaris is a common inflammatory skin condition affecting the pilosebaceous units, characterized by comedones, papules, pustules, nodules, and cysts. While traditionally viewed as a localized skin disorder, mounting evidence suggests that acne has systemic connections, particularly with the gut microbiome.[1]
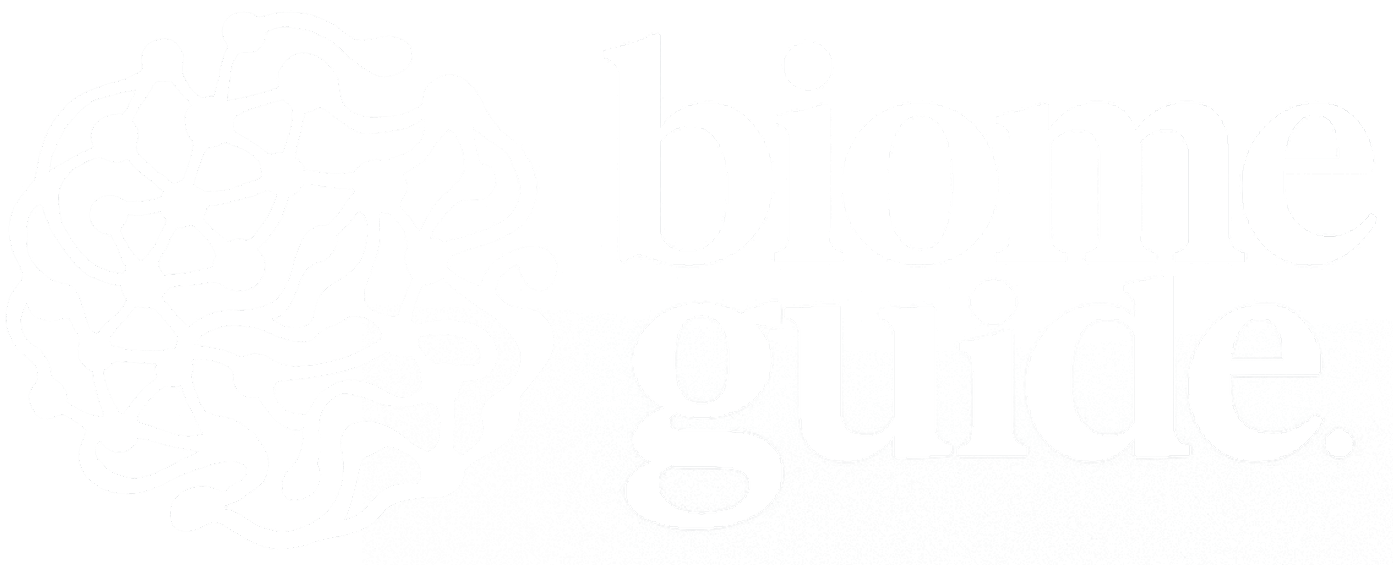
The gut-skin axis represents a bidirectional communication system where gut health significantly impacts skin conditions.[2] Research has demonstrated that gut dysbiosis (microbial imbalance) can contribute to systemic inflammation, altered immune responses, and increased intestinal permeability—all factors that may exacerbate acne.
How Gut Dysbiosis Influences Acne Development
Several mechanisms link gut microbiome imbalances to acne pathogenesis:[2]
Systemic Inflammation
Gut dysbiosis can trigger the release of pro-inflammatory cytokines that circulate throughout the body, potentially exacerbating inflammatory skin conditions like acne.
Intestinal Permeability
Increased intestinal permeability ("leaky gut") allows bacterial products and toxins to enter the bloodstream, triggering immune responses that may manifest as skin inflammation.
Altered Hormone Metabolism
Gut microbes influence the metabolism of hormones, including androgens, which play a significant role in sebum production and acne development.
Nutrient Absorption
Gut dysbiosis can impair the absorption of nutrients essential for skin health, such as zinc, vitamin A, and omega-3 fatty acids.
Key Microorganisms in Acne
Both gut and skin microbiomes play important roles in acne development.[3] Clinical trials with both topical and oral probiotics have shown positive results in acne treatment, especially through modulation of the intestinal microbiota, generating an anti-inflammatory response and restoring intestinal integrity.[4]
Gut Microbiome
- Beneficial bacteria: Lactobacillus and Bifidobacterium species help maintain gut barrier integrity and modulate immune responses
- Problematic bacteria: Overgrowth of certain Firmicutes and reduced Bacteroidetes diversity have been associated with inflammatory conditions
Skin Microbiome
- Cutibacterium acnes (formerly Propionibacterium acnes): While a normal component of skin microbiota, certain strains and overgrowth are associated with acne development. However, research shows this bacterium is also present in healthy skin, suggesting that strain-specific differences and overall microbial balance play crucial roles.[5]
- Staphylococcus epidermidis: May play a protective role by inhibiting C. acnes growth and inflammation
- Malassezia species: These fungi can contribute to inflammatory responses in some individuals
Microbiome-Based Approaches for Acne Management
Emerging research supports several microbiome-focused strategies for managing acne:[6]
Oral Probiotics
Clinical studies have shown that certain probiotic strains, particularly Lactobacillus and Bifidobacterium species, can reduce acne severity by:[7]
- Reducing systemic inflammation
- Improving gut barrier function
- Modulating immune responses
- Regulating sebum production
Evidence Level: Moderate
Topical Probiotics
Applying beneficial bacteria directly to the skin may help:
- Inhibit C. acnes growth
- Reduce inflammation
- Restore skin microbiome balance
- Strengthen the skin barrier
Evidence Level: Preliminary to Moderate
Dietary Modifications
Several dietary approaches may improve both gut microbiome health and acne:
- Low glycemic diet: Reduces insulin and IGF-1 levels, which can decrease sebum production
- Mediterranean diet: Rich in anti-inflammatory compounds and prebiotic fibers
- Omega-3 fatty acids: Help reduce inflammation and may improve acne
- Prebiotic-rich foods: Nourish beneficial gut bacteria
Evidence Level: Moderate to Strong
Prebiotics
Dietary fibers that selectively feed beneficial gut bacteria can improve gut health and potentially reduce acne severity.
Evidence Level: Preliminary

The Gut-Brain-Skin Axis
The connection between acne and the microbiome extends beyond just the gut-skin axis to include the brain, forming what researchers call the gut-brain-skin axis.[1] Psychological stress can:
- Alter gut microbiome composition
- Increase intestinal permeability
- Trigger inflammatory responses
- Exacerbate acne
This explains why stress management techniques and addressing psychological factors can be important components of comprehensive acne treatment.
Clinical Evidence and Research Highlights
Recent studies have provided compelling evidence for the gut-skin connection in acne:
A 2018 study found that acne patients had significantly different gut microbiome compositions compared to healthy controls, with reduced diversity and beneficial bacteria.[3]
A 2016 randomized controlled trial showed that Lactobacillus rhamnosus SP1 supplementation normalized skin gene expression related to insulin signaling and improved adult acne.[8]
A 2013 study demonstrated that combining probiotics with antibiotic therapy improved acne outcomes compared to antibiotics alone.[7]
Personalized Approaches to Acne Management
Given the complex interplay between individual microbiome compositions, genetics, diet, and lifestyle factors, personalized approaches to acne management are likely to be most effective:
- Microbiome testing: Analyzing both gut and skin microbiomes can identify specific imbalances
- Targeted probiotics: Selecting specific strains based on individual needs
- Personalized dietary recommendations: Tailoring nutritional advice based on microbiome composition and food sensitivities
- Combination therapies: Integrating conventional treatments with microbiome-focused approaches
Future Directions in Microbiome-Based Acne Treatment
The field of microbiome research in acne is rapidly evolving, with several promising developments on the horizon. Research underscores the complexity of microbial involvement in acne pathogenesis and delineates the effects of acne therapeutics on microbial diversity, abundance, and composition, emphasizing the necessity for personalized approaches in acne management based on microbiome modulation.[5]
- Strain-specific probiotics: Formulations targeting specific microbial imbalances associated with acne
- Precision prebiotics: Compounds designed to selectively nourish beneficial bacteria depleted in acne patients
- Bacteriophage therapy: Viruses that specifically target problematic C. acnes strains while sparing beneficial ones
- Postbiotics: Beneficial bacterial metabolites that may provide skin benefits without requiring live organisms
- Mendelian randomization studies: Recent research has identified causal relationships between specific gut microbes like Bifidobacterium and acne through mediation analysis involving DHA and degree of unsaturation.[9]
Key Takeaways
- Acne has significant connections to gut microbiome health through the gut-skin axis[2]
- Gut dysbiosis can contribute to systemic inflammation, altered immune responses, and increased intestinal permeability, all of which may exacerbate acne
- Both oral and topical probiotics show promise for acne management[6]
- Dietary modifications that support gut health may improve acne symptoms
- Personalized approaches targeting individual microbiome compositions are likely to be most effective
- Emerging research is paving the way for more targeted, microbiome-focused acne treatments
Research Summary
Emerging research has established connections between gut microbiome composition and skin health, with studies showing that gut dysbiosis can contribute to systemic inflammation and skin conditions like acne. Probiotic interventions have shown promise in clinical trials for improving both gut health and acne symptoms.
References
- Bowe WP, Logan AC.. Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future?. Gut Pathogens. 2011;3(1):1. doi:10.1186/1757-4749-3-1 ↩
- Salem I, Ramser A, Isber N, Tober A.. The gut microbiome as a major regulator of the gut-skin axis. Frontiers in Microbiology. 2018;9:1459. doi:10.3389/fmicb.2018.01459 ↩
- Deng Y, Wang H, Zhou J, Mou Y, Wang G, Xiong X.. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Dermato-Venereologica. 2018;98(8):783-790. doi:10.2340/00015555-2968 ↩
- Sánchez-Pellicer P, Navarro-López L, Núñez-Delegido A, et al.. Influence of the Microbiota and Probiotics in Acne: A Narrative Review. Microorganisms. 2022;10(7):1303. doi:10.3390/microorganisms10071303 ↩
- Podwojniak A, Tan IJ, Sauer J, et al.. Acne and the cutaneous microbiome: A systematic review of mechanisms and implications for treatments. Journal of the European Academy of Dermatology and Venereology. 2025;39(4):793-805. doi:10.1111/jdv.20332 ↩
- Kober MM, Bowe WP.. The effect of probiotics on immune regulation, acne, and photoaging. International Journal of Women's Dermatology. 2015;1(2):85-89. doi:10.1016/j.ijwd.2015.02.001 ↩
- Jung GW, Tse JE, Guiha I, Rao J.. Prospective, randomized, open-label trial comparing the safety, efficacy, and tolerability of an acne treatment regimen with and without a probiotic supplement and minocycline in subjects with mild to moderate acne. Journal of Cutaneous Medicine and Surgery. 2013;17(2):114-122. doi:10.2310/7750.2012.12026 ↩
- Fabbrocini G, Bertona M, Picazo Ó, Pareja-Galeano H, Monfrecola G, Emanuele E.. Supplementation with Lactobacillus rhamnosus SP1 normalises skin expression of genes implicated in insulin signalling and improves adult acne. Beneficial Microbes. 2016;7(5):625-630. doi:10.3920/BM2016.0089 ↩
- He X, Zhang Z, Jiang H, et al.. Causal association of gut microbes and blood metabolites with acne identified through systematic mendelian randomization. Scientific Reports. 2024;14:26816. doi:10.1038/s41598-024-78603-z ↩