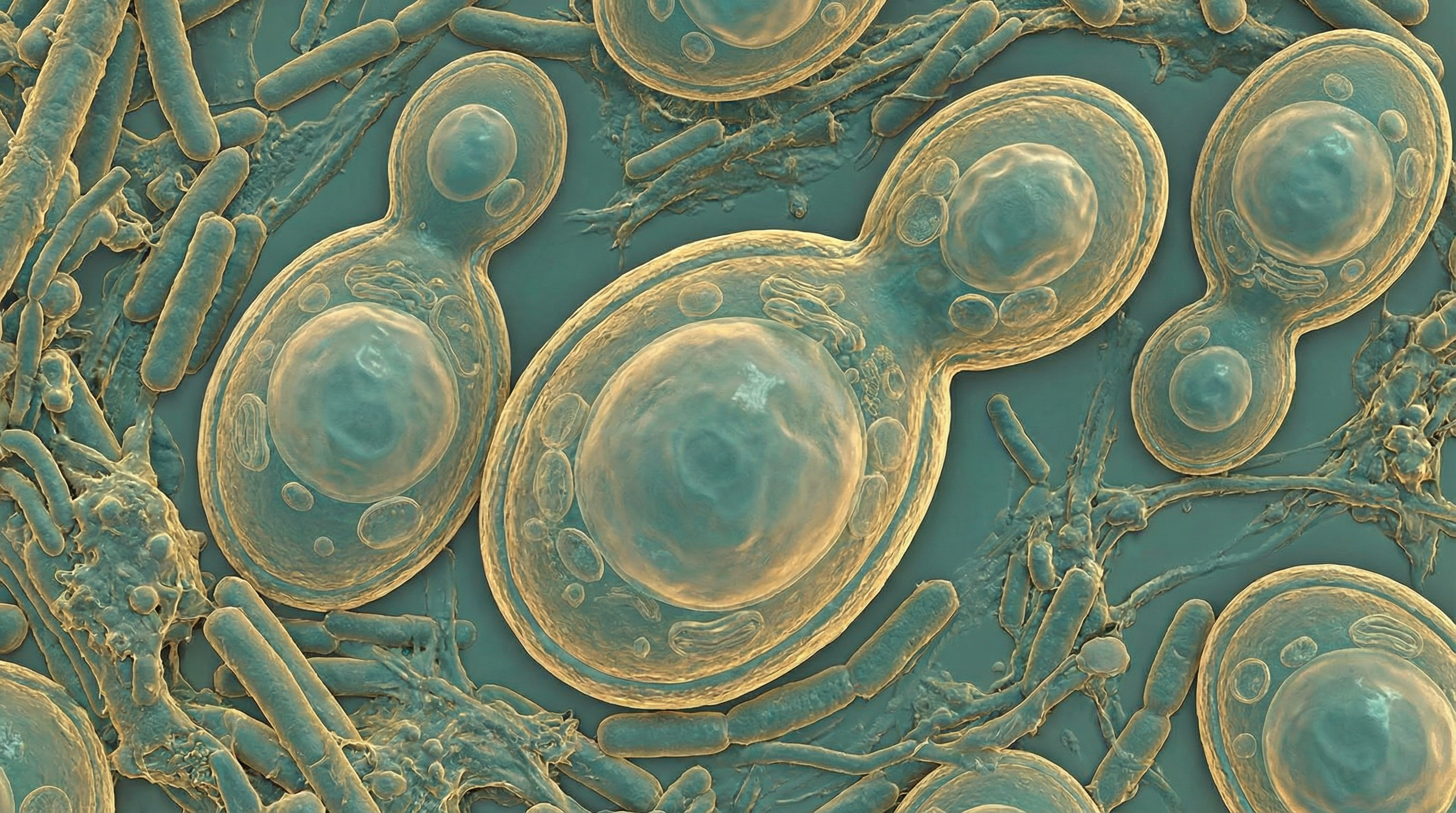
Saccharomyces boulardii is a non-pathogenic probiotic yeast, first isolated from lychee and mangosteen fruit in the 1920s by Henri Boulard. The most studied strain, CNCM I-745, is the only yeast widely used as a probiotic for gastrointestinal health, with extensive clinical evidence supporting its efficacy in preventing and treating various diarrheal conditions.
Mechanisms of Action
S. boulardii exerts its beneficial effects through multiple, well-characterized mechanisms that target both pathogens and host immune responses.
Anti-Toxin Effects
A key mechanism involves direct proteolytic cleavage of bacterial toxins. S. boulardii secretes a 54 kDa serine protease that cleaves Clostridium difficile toxins A and B, reducing toxin A receptor binding by 42% and inhibiting ileal secretion by 46%. The yeast also blocks MAP kinase activation, with studies showing it blocks ERK1/2 and JNK/SAPK pathways, reducing toxin A-induced KC cytokine from 1,390 pg/mg to 426 pg/mg (p < 0.001).
Additional toxin-neutralizing capabilities include:
- A 120 kDa protein that inhibits cholera toxin-induced chloride secretion
- A 63 kDa alkaline phosphatase that dephosphorylates E. coli LPS endotoxins
- Cleavage of Bacillus anthracis lethal toxin
Trophic Effects on Enterocytes
S. boulardii promotes intestinal epithelial health through secretion of polyamines (spermine, spermidine, putrescine) that enhance protein synthesis, RNA stabilization, and enterocyte maturation. It stimulates brush border enzyme production including disaccharidases, lipase, and trypsin.
Cell migration studies demonstrate remarkable effects: S. boulardii-treated cells show migration rates of 80 μm/hour vs. 40 μm/hour in controls, with in vivo BrdU-labeled enterocytes reaching 45% of villus height vs. 20% in controls. This occurs through activation of α2β1 integrin collagen receptors and MAPK/ERK1/2 pathways.
Immunomodulation
S. boulardii profoundly modulates dendritic cell function and T cell responses. In IBD patients, it significantly reduces CD40 expression on myeloid dendritic cells (from 93.61% to 47.58% in Crohn's remission, p < 0.01) and inhibits T cell proliferation (45.6% to 27.77%, p < 0.01).
Key immunological effects include:
- Pro-inflammatory reduction: TNF-α reduced from 315.9 to 118.8 pg/mL in LPS-stimulated dendritic cells (p < 0.01)
- Anti-inflammatory enhancement: Increased IL-10 and IL-4 production
- Secretory IgA stimulation: Enhanced anti-toxin antibody production (IgA, IgM, IgG)
- NF-κB pathway inhibition: Blocks NF-κB activation and translocation
Clinical Evidence
Antibiotic-Associated Diarrhea Prevention
Meta-analyses provide strong evidence for AAD prevention. A 2015 meta-analysis of 21 RCTs (4,780 participants) found S. boulardii reduced AAD from 18.7% to 8.5%, with RR 0.47 (95% CI: 0.38-0.57) and NNT of 10.
The JAMA 2012 meta-analysis of 82 RCTs confirmed these findings, showing Saccharomyces-based probiotics achieved RR 0.48 (95% CI: 0.35-0.65), superior to Lactobacillus-based products (RR 0.64). A key advantage is resistance to antibiotics, allowing co-administration during antibiotic therapy.
Clostridioides difficile Infection
For CDI recurrence prevention, S. boulardii demonstrates significant benefit. A 2025 RCT of 120 patients showed adding S. boulardii to vancomycin reduced recurrence from 13.11% to 1.69% (p = 0.032), with global cure rates of 96.61% vs. 85.25% (p = 0.044).
Meta-analysis of 6 RCTs shows RR 0.59 (95% CI: 0.41-0.85, p = 0.005) for recurrence prevention, with greatest efficacy when combined with high-dose vancomycin.
Acute Infectious Diarrhea
In pediatric acute diarrhea, a multicenter RCT of 100 children showed S. boulardii reduced time to recovery from 95.3 hours to 65.8 hours (difference: -29.5h, p = 0.0001), with 82.6% recovery at 3 days vs. 16.3% with placebo.
For rotavirus-specific diarrhea, median duration decreased from 89 hours to 60 hours with significant reduction in hospitalization.
Traveler's Diarrhea Prevention
Clinical trials show dose-dependent protection:
- Placebo: 39-43% diarrhea rate
- 250 mg S. boulardii: 32-34% (p < 0.05)
- 1 g S. boulardii: 29% (p < 0.05)
Other Clinical Applications
- H. pylori eradication: Increases eradication rates from 71% to 80%, reduces side effects including epigastric distress (14.5% vs. 43.5%, p < 0.05)
- HIV-related diarrhea: 61% resolution vs. 12% placebo (p = 0.002)
- Ulcerative colitis: Pilot data shows 70.8% achieving clinical remission when added to mesalazine
Safety Profile
General Safety
S. boulardii is generally well-tolerated with common mild side effects including intestinal gas, thirst, and bloating. Adverse event rates in clinical trials are typically similar to or lower than placebo.
Fungemia Risk
Saccharomyces fungemia is a rare but serious complication requiring careful patient selection. Key risk data:
- 40% of invasive Saccharomyces infections associated with S. boulardii use
- Case fatality rate: 22% at day 7, 37% at day 28
- Odds ratio for fungemia: 14 (95% CI: 4-44) compared to controls
High-risk populations (contraindications):
- Patients with central venous catheters
- Immunocompromised patients
- Critically ill/ICU patients
- Severe IBD with mucosal disruption
- Recent GI surgery
Environmental transmission can occur through airborne spread when opening packets, with organisms persisting on surfaces up to 2 hours and on healthcare worker hands for 30 minutes.
Dosing Recommendations
| Indication | Dose | Duration |
|---|---|---|
| AAD Prevention | 250-500 mg twice daily | Throughout antibiotics + 5-7 days after |
| CDI Recurrence | 250 mg twice daily | 10+ days with antibiotics |
| Acute Diarrhea | 250-1000 mg/day | 5 days |
| Traveler's Prophylaxis | 250-1000 mg/day | Duration of trip |
Optimal efficacy typically requires >10^9 organisms/day (approximately 5 billion CFU). Lyophilized preparations are preferred over heat-dried for cell viability.
Unique Advantages
S. boulardii offers several advantages over bacterial probiotics:
- Antibiotic resistance: Can be co-administered with any antibiotic
- Acid stability: Survives gastric passage without enteric coating
- Multiple mechanisms: Anti-toxin, trophic, and immunomodulatory effects
- Transient colonization: Cleared within days of discontinuation, reducing long-term effects
- Does not alter healthy microbiota: Preserves commensal composition without challenge
Microbiota Interactions
While S. boulardii does not permanently colonize, it supports microbiome health:
- Accelerates steady-state recovery after antibiotics (10 days vs. 22 days in controls)
- Increases Lachnospiraceae and Ruminococcaceae (SCFA producers)
- Limits rise of Enterobacteriaceae and Clostridiaceae during dysbiosis
- Binds pathogens (E. coli, Salmonella) to yeast cell wall for elimination
Conclusions
Saccharomyces boulardii represents the best-studied probiotic yeast with robust clinical evidence supporting its use in preventing antibiotic-associated diarrhea, reducing CDI recurrence, and treating acute infectious diarrhea. Its multiple mechanisms of action, antibiotic resistance, and favorable safety profile in appropriate populations make it a valuable therapeutic option. However, strict attention to contraindications—particularly central venous catheters and immunocompromise—is essential given the risk of fungemia in vulnerable patients.
