Improved Vaccine Response
Enhance your immune system's ability to respond to vaccinations and build lasting protection through microbiome optimization.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Microbiome-Vaccine Connection
Vaccines are one of medicine's greatest achievements, but their effectiveness varies significantly between individuals. Research has revealed that your gut microbiome plays a crucial role in determining how well you respond to vaccines—affecting both the magnitude and duration of protective immunity[3].
Understanding this connection opens new possibilities for optimizing vaccine responses through microbiome-supporting strategies, particularly important for vulnerable populations who may not respond optimally to vaccination.
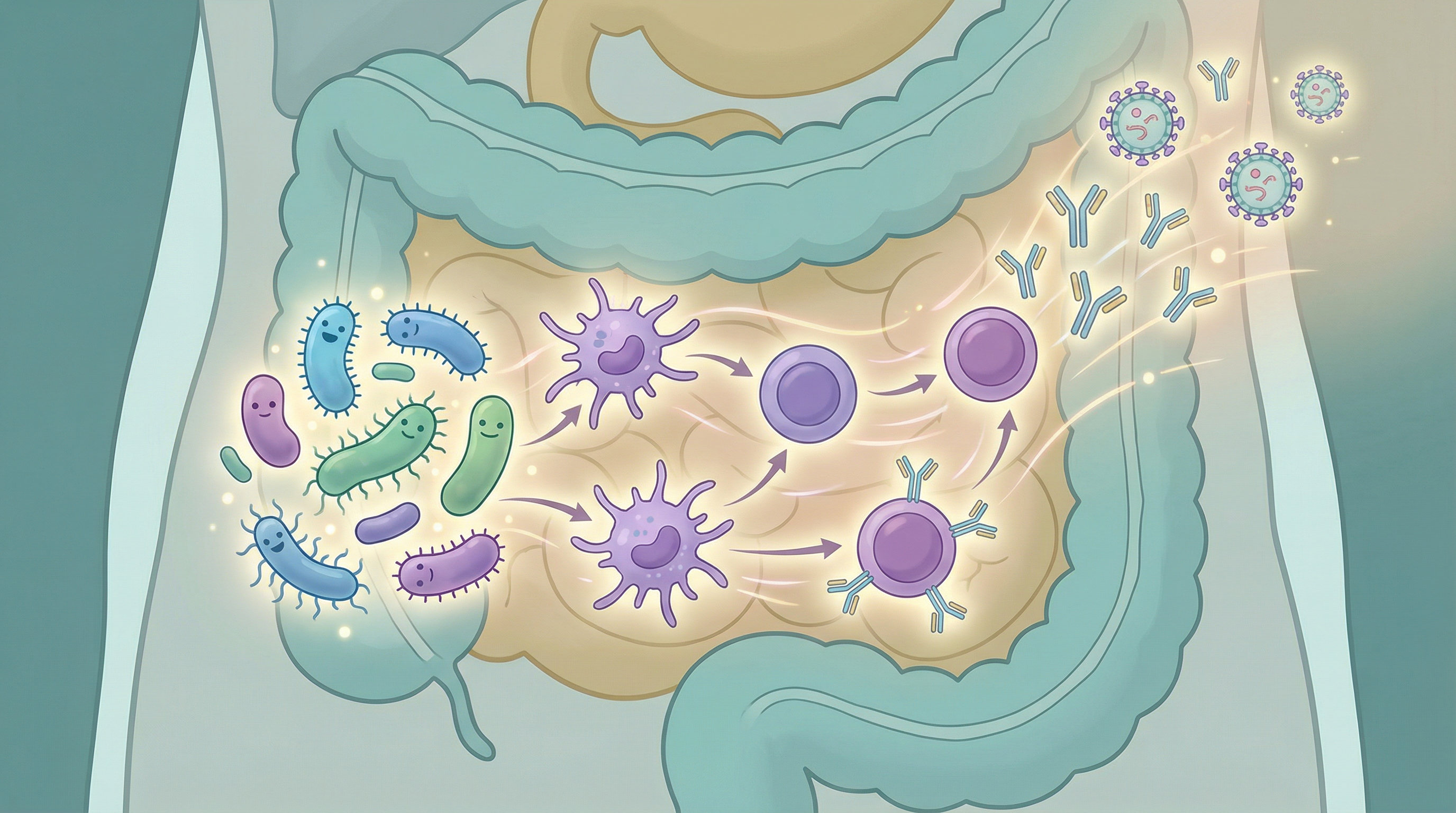
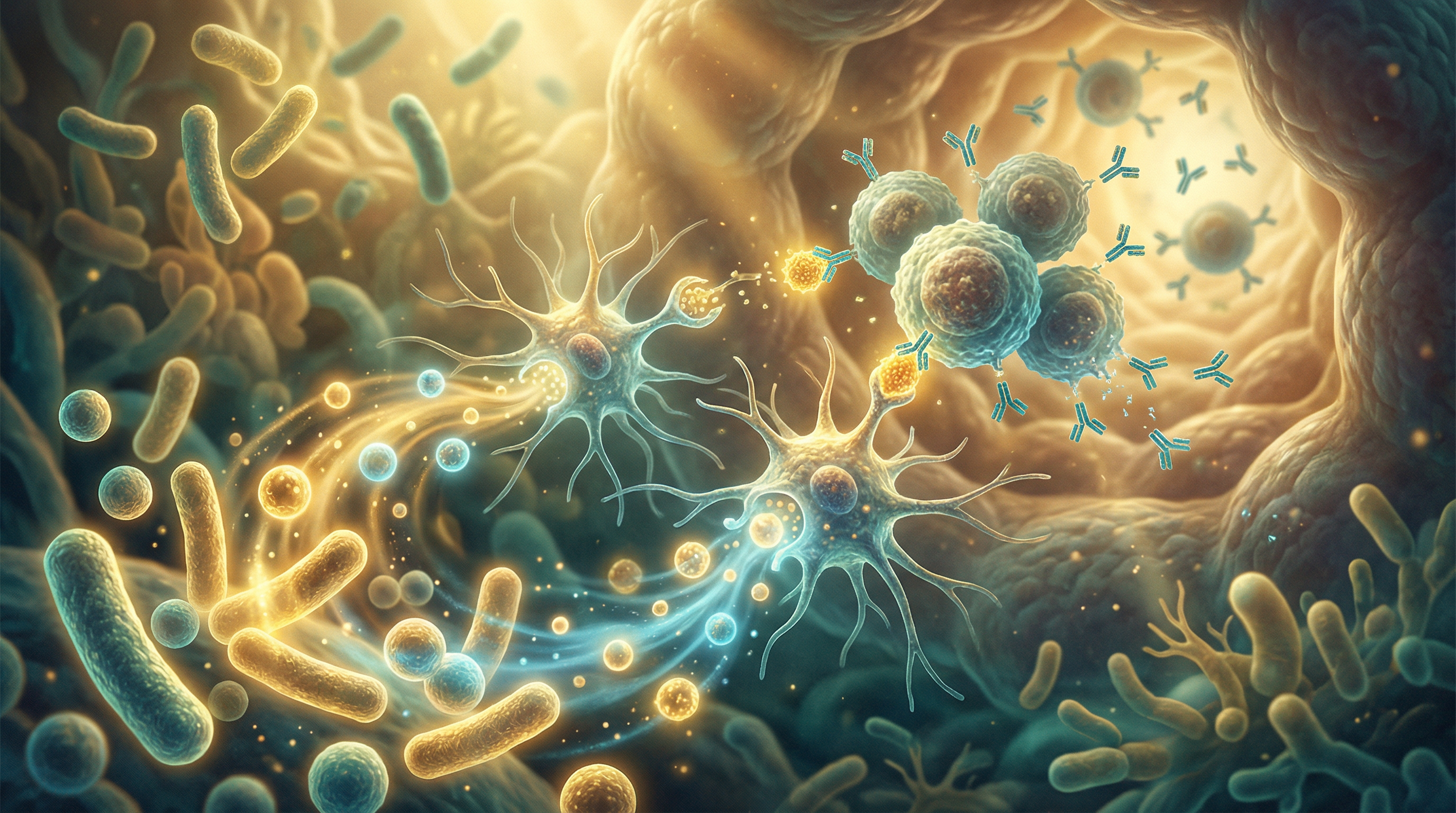
How Gut Bacteria Influence Vaccine Response
Immune Cell Priming
The microbiome keeps your immune system in a state of readiness[1]:
Baseline activation:
- Beneficial bacteria provide constant, low-level immune stimulation
- This maintains immune cells in an alert, responsive state
- Without this priming, responses to vaccines are weaker
Adjuvant-like effects:
- Certain bacterial components naturally enhance immune responses
- They can amplify the signals generated by vaccines
- This leads to stronger antibody production
A comprehensive review of the literature confirms that the intestinal microbiome has significant effects on both oral and parenteral vaccine responses[5].
B Cell Function
B cells produce antibodies, and the microbiome influences their activity:
- Gut bacteria affect B cell development and maturation
- They influence class-switching, which determines antibody type
- Microbiome diversity correlates with antibody diversity
- Better B cell function means more effective vaccine responses
T Cell Support
T cells coordinate immune responses and the microbiome shapes their function[6]:
Helper T cells:
- Necessary for robust antibody production
- Their proper development requires microbial signals
- Support long-lasting immune memory
Memory T cells:
- Critical for long-term vaccine protection
- Microbiome influences their formation and maintenance
- Better memory means longer-lasting immunity
Dendritic Cell Activation
These cells bridge innate and adaptive immunity:
- They present vaccine antigens to T cells
- Microbiome signals affect their activation state
- Better-activated dendritic cells lead to stronger responses
Evidence: Microbiome and Vaccine Outcomes
The Antibiotic Study
Landmark research demonstrated the microbiome's importance[1]:
- Healthy adults received antibiotics before flu vaccination
- Those with disrupted microbiomes had significantly reduced responses
- The effect was most pronounced in those with low pre-existing immunity
- Recovery of full vaccine response required microbiome restoration
Infant Vaccination
Early-life microbiome matters for childhood vaccines[2]:
- Babies with more diverse microbiomes respond better to vaccines
- Bifidobacterium abundance correlates with vaccine responses
- Antibiotic exposure in infancy can impair vaccination effectiveness
- Breastfeeding, which shapes the infant microbiome, supports vaccine responses
Geographic Variations
Vaccine responses vary dramatically by region, and research in rural Ghana demonstrated significant correlation between infant gut microbiome composition and rotavirus vaccine response[4]:
- Children in developing countries often respond less well to oral vaccines
- This correlates with differences in microbiome composition
- Environmental enteropathy affects gut bacteria and vaccine responses
- Microbiome interventions may help bridge this gap
Key Microbes for Vaccine Response
Bifidobacterium longum
Consistently associated with better vaccine outcomes:
- Abundant in healthy infants who respond well to vaccines
- Produces metabolites that support immune function
- Associated with better influenza vaccine responses
- Supports overall immune system development
Lactobacillus rhamnosus
Well-studied for immune enhancement:
- Has been shown to improve responses to multiple vaccines
- Supports both antibody and cellular immunity
- May extend the duration of vaccine protection
- Safe and well-tolerated as a supplement
Bifidobacterium animalis
Another beneficial species for immunity:
- Associated with robust vaccine responses
- Supports intestinal barrier function
- Produces immune-modulating metabolites
- Commonly found in yogurt and fermented dairy
Prevotella Species
Important for adult vaccine responses:
- Associated with better influenza vaccine outcomes
- More abundant in people with high-fiber diets
- May indicate overall microbiome health
- Thrive on plant-based dietary patterns

Factors That Impair Vaccine Responses
Understanding what weakens responses helps you optimize them:
Antibiotic Use
- Recent antibiotics significantly reduce vaccine effectiveness[1]
- The effect can last for months after treatment
- When possible, time vaccinations away from antibiotic courses
- If antibiotics are necessary, focus on microbiome recovery afterward
Poor Diet
- Low-fiber diets reduce beneficial bacteria
- Processed foods may promote inflammatory species
- Nutrient deficiencies impair immune function
- Dietary changes before vaccination can help
Chronic Stress
- Stress hormones alter microbiome composition
- Impairs immune cell function
- Reduces antibody production
- Stress management supports vaccine responses
Sleep Deprivation
- Poor sleep reduces vaccine effectiveness
- Affects immune cell activation
- Disrupts microbiome circadian rhythms
- Prioritize sleep around vaccination time
Advanced Age
- The aging microbiome becomes less diverse
- Immune function naturally declines
- However, microbiome optimization can partially compensate
- Older adults may benefit most from microbiome support
Optimizing Your Microbiome for Vaccination
Two Weeks Before
Dietary preparation:
- Increase fiber intake gradually
- Include diverse plant foods
- Add fermented foods daily
- Reduce processed foods and sugar
Lifestyle adjustments:
- Prioritize sleep (7-9 hours)
- Manage stress actively
- Maintain moderate exercise
- Avoid unnecessary antibiotics
Day of Vaccination
Best practices:
- Ensure you're well-rested
- Eat a balanced meal
- Stay hydrated
- Try to be relaxed and calm
What to avoid:
- Heavy alcohol consumption
- Extreme stress
- Sleep deprivation
- Intense exercise
Two Weeks After
Continue supporting your microbiome:
- Maintain high fiber intake
- Keep eating fermented foods
- Get quality sleep
- This supports the immune response development
Allow time for response:
- Antibody production peaks at 2-4 weeks
- Memory cell development takes longer
- Continue healthy practices during this window
Specific Populations
Older Adults
May benefit especially from:
- Probiotic supplementation before vaccination
- Higher fiber intake
- Adequate protein for immune function
- Vitamin D optimization
Immunocompromised Individuals
Should consider:
- Working with healthcare providers on timing
- Microbiome testing to identify deficiencies
- Targeted probiotic interventions
- Longer preparation periods
Children
Parents can support vaccine responses by[4]:
- Maintaining breastfeeding if possible
- Introducing diverse solid foods
- Limiting unnecessary antibiotics
- Including fermented foods age-appropriately
The Future of Vaccine Enhancement
Research is exploring:
- Synbiotic adjuvants: Probiotic/prebiotic combinations given with vaccines
- Microbiome-based vaccine design: Vaccines that leverage gut bacteria
- Personalized approaches: Tailoring strategies based on individual microbiomes
- Targeted interventions: Specific strains for specific vaccines
Building Better Vaccine Responses
Supporting your microbiome for optimal vaccination involves:
- Maintaining year-round microbiome health through diet and lifestyle
- Intensifying support in the weeks around vaccination
- Avoiding microbiome-disrupting factors when possible
- Understanding that this is one factor among many affecting vaccine responses
While microbiome optimization won't guarantee perfect vaccine responses, evidence suggests it can meaningfully improve outcomes, particularly for those who might otherwise respond suboptimally.
Supporting Practices
Evidence-based strategies to support this benefit:
- Ensure adequate fiber intake before and after vaccination
- Include fermented foods to support immune-training bacteria
- Get quality sleep, especially around vaccination time
- Manage stress which can impair vaccine responses
- Avoid antibiotics around vaccination when possible
- Stay hydrated and maintain good nutrition
References
- Hagan T, Cortese M, Ber N, et al.. Antibiotics-Driven Gut Microbiome Perturbation Alters Immunity to Vaccines in Humans. Cell. 2019;178(6):1313-1328. doi:10.1016/j.cell.2019.08.010
- Lynn MA, Tumes DJ, Choo JM, et al.. Early-Life Antibiotic-Driven Dysbiosis Leads to Dysregulated Vaccine Immune Responses in Mice. Cell Host & Microbe. 2022;29(4):565-582. doi:10.1016/j.chom.2021.01.016
- Ciabattini A, Olivieri R, Lazzeri E, Medaglini D. Role of the Microbiota in the Modulation of Vaccine Immune Responses. Frontiers in Microbiology. 2019;10:1305. doi:10.3389/fmicb.2019.01305
- Harris VC, Armah G, Fuentes S, et al.. Significant Correlation Between the Infant Gut Microbiome and Rotavirus Vaccine Response in Rural Ghana. The Journal of Infectious Diseases. 2017;215(1):34-41. doi:10.1093/infdis/jiw518
- Zimmermann P, Curtis N. The influence of the intestinal microbiome on vaccine responses. Vaccine. 2018;36(30):4433-4439. doi:10.1016/j.vaccine.2018.04.066
- Parkin J, Cohen B. An overview of the immune system. The Lancet. 2001;357(9270):1777-1789. doi:10.1016/S0140-6736(00)04904-7
