Strengthened Mucosal Immunity
Fortify your body's mucosal surfaces—gut, respiratory, and urogenital—through microbiome-supported immune function for comprehensive protection.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
Understanding Mucosal Immunity
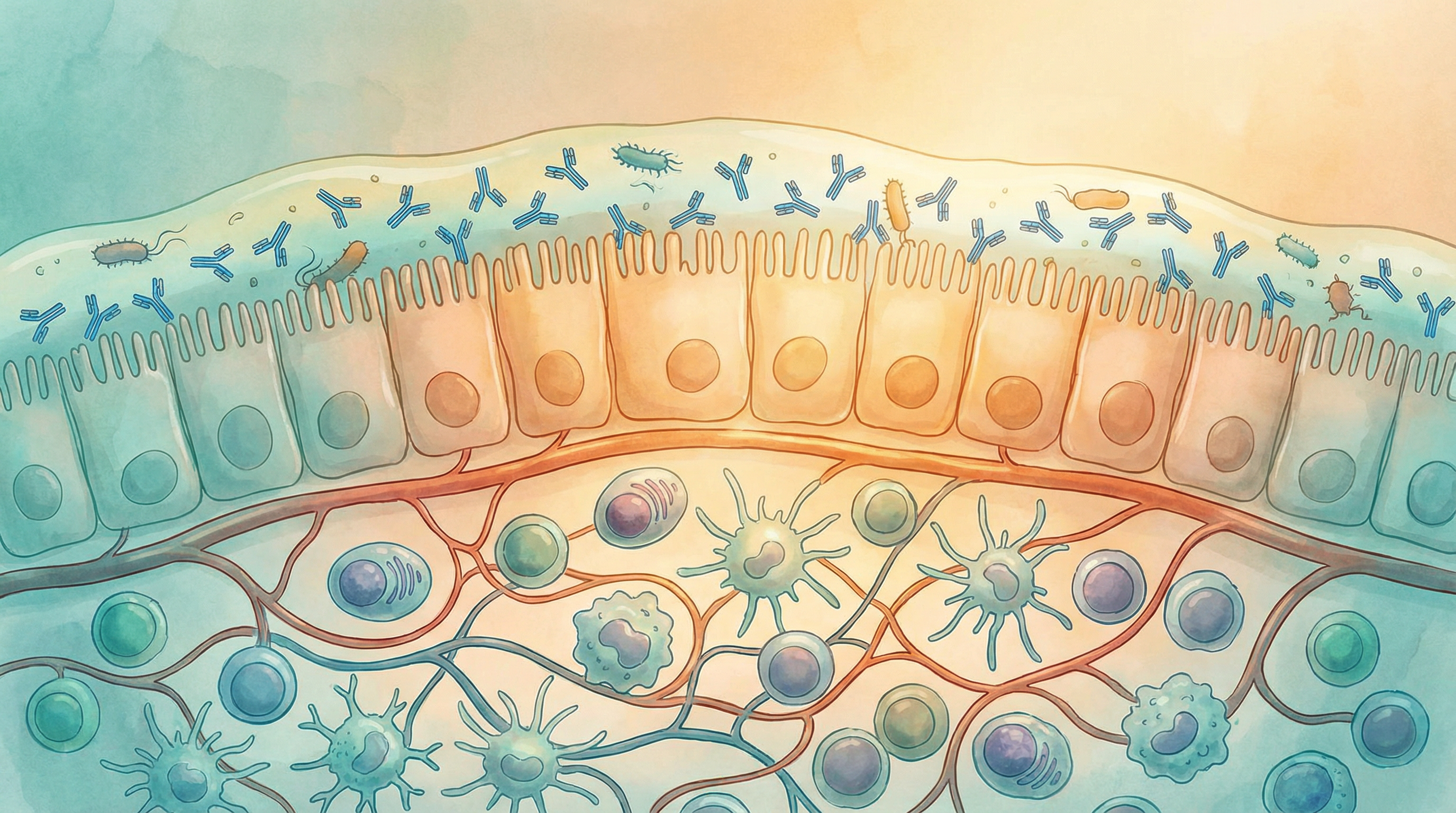
Your body's mucosal surfaces represent the primary interface with the external environment. These surfaces—lining your gut, respiratory tract, urogenital system, and eyes—are where most pathogens attempt to enter. A specialized branch of the immune system, mucosal immunity, has evolved to protect these vulnerable areas[1].
What's remarkable is how deeply the microbiome influences mucosal immune function. The bacteria living on these surfaces don't just coexist with the immune system—they actively shape and strengthen it.
The Mucosal Immune System
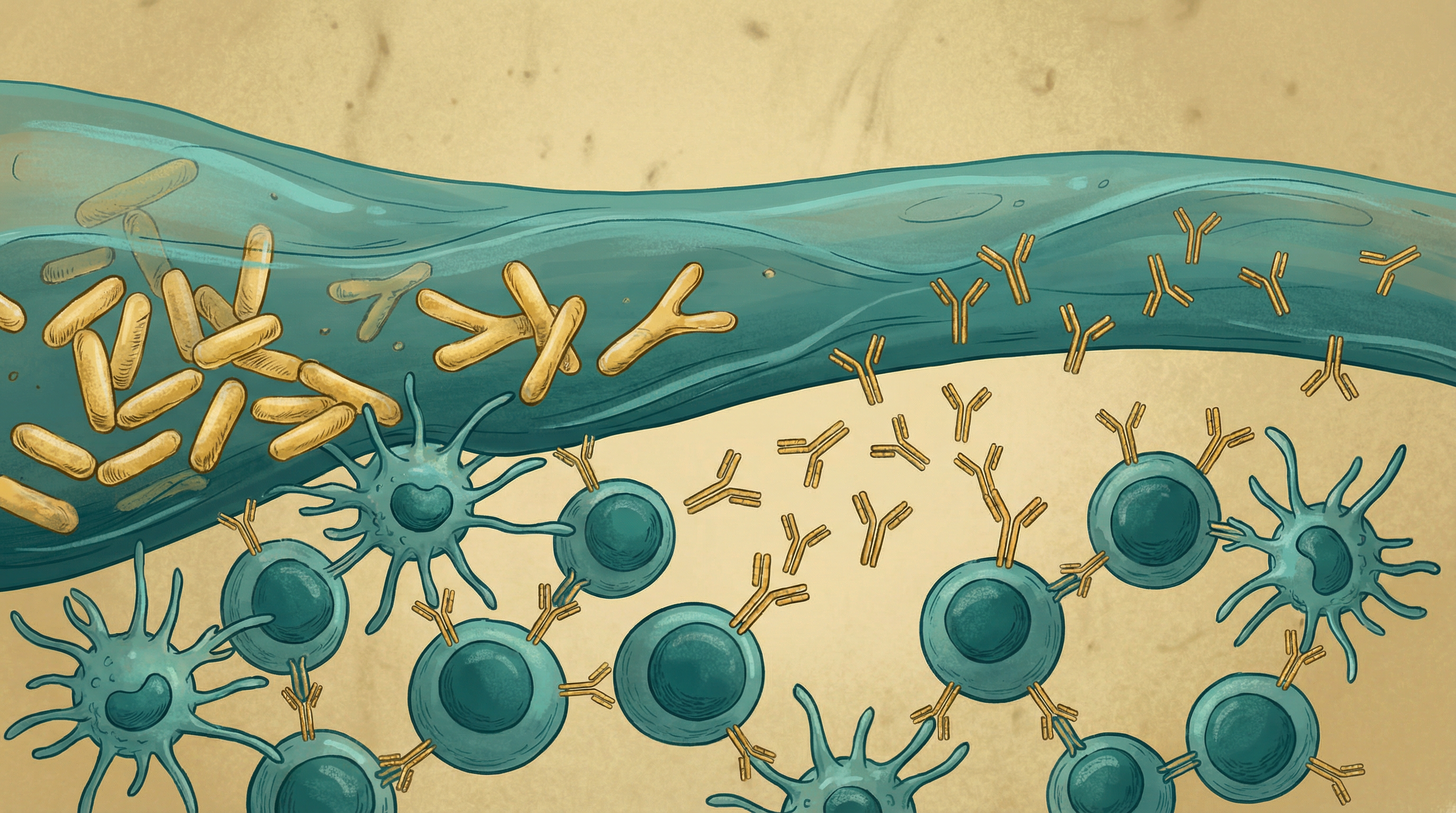
Secretory IgA: The First Line of Defense
Secretory IgA (sIgA) is the dominant antibody at mucosal surfaces[3]:
Functions:
- Coats bacteria and viruses to prevent attachment
- Neutralizes toxins before they can cause harm
- Traps pathogens in mucus for removal
- Maintains balance with beneficial bacteria
Microbiome dependence:
- Germ-free animals produce very little sIgA
- Specific bacteria trigger sIgA production
- The quality and specificity of sIgA depends on microbial exposure
- A diverse microbiome leads to more comprehensive sIgA coverage
Mucosal Associated Lymphoid Tissue (MALT)
Specialized immune structures exist throughout mucosal surfaces:
Gut-associated lymphoid tissue (GALT):
- Peyer's patches sample intestinal contents
- Mesenteric lymph nodes coordinate gut immune responses
- Contains most of the body's immune cells
Nasal-associated lymphoid tissue (NALT):
- Protects the respiratory tract entry point
- Includes tonsils and adenoids
- Connected to the broader mucosal immune network
Bronchus-associated lymphoid tissue (BALT):
- Develops in response to respiratory infections
- Provides local immune protection in the lungs
The Common Mucosal Immune System
Remarkably, stimulating immunity at one mucosal site can protect others[2]:
- Immune cells educated in the gut can travel to respiratory surfaces
- This explains how oral probiotics can help with respiratory infections
- The gut microbiome influences immunity throughout the body
- This interconnection makes gut health central to overall mucosal protection
How the Microbiome Strengthens Mucosal Immunity
Immune Cell Development
Mucosal tissues contain specialized immune cells shaped by bacteria[4]:
Intraepithelial lymphocytes:
- Positioned between mucosal cells
- Provide rapid local defense
- Their development requires microbial signals
IgA-producing plasma cells:
- Make the antibodies that protect mucosal surfaces
- Require bacterial stimulation for proper development
- Their diversity reflects microbiome diversity
Regulatory cells:
- Prevent excessive reactions to harmless substances
- Maintain tolerance to food and beneficial bacteria
- Reduce risk of allergies and autoimmunity
The complex interplay between the gut microbiota and the immune system has been characterized as both "friends and foes," with proper balance being essential for health[6].
Antimicrobial Peptide Production
Mucosal cells produce natural antibiotics in response to bacteria:
- Defensins target harmful bacteria while sparing beneficial ones
- Cathelicidins have broad antimicrobial activity
- Lysozyme breaks down bacterial cell walls
- Production depends on appropriate microbial signals
Mucus Layer Maintenance
The mucus barrier works with the immune system:
- Traps pathogens for removal
- Provides a habitat for beneficial bacteria
- Contains sIgA and antimicrobial peptides
- Is maintained partly through microbial signals
Key Microbes for Mucosal Immunity
Lactobacillus rhamnosus
Extensively studied for mucosal immune support:
- Enhances sIgA production
- Reduces duration of respiratory infections
- Supports gut barrier function
- Modulates inflammatory responses at mucosal surfaces
Bifidobacterium lactis
Important for mucosal immune development:
- Supports sIgA responses
- Associated with reduced respiratory infections
- Helps maintain healthy mucosal barriers
- Safe for all ages including infants
Lactobacillus plantarum
Versatile mucosal immune supporter:
- Produces antimicrobial compounds
- Enhances barrier function
- Supports balanced immune responses
- Found in many fermented vegetables
Streptococcus salivarius
A key member of the oral and respiratory microbiome:
- Naturally colonizes mouth and throat
- Produces bacteriocins against pathogens
- Competes with harmful bacteria
- Specific strains (K12, M18) used as oral probiotics
The Gut-Lung Axis
The connection between gut and respiratory immunity is particularly important[5]:
Bidirectional Communication
- Gut bacteria influence lung immune cells
- Respiratory infections can alter gut microbiome
- Immune cells travel between gut and lungs
- Metabolites from gut bacteria reach the lungs via circulation
Respiratory Infection Protection
Studies show gut microbiome influences respiratory health:
- Diverse gut microbiomes associated with fewer respiratory infections
- Probiotics can reduce incidence and duration of colds
- Antibiotic-induced gut disruption increases pneumonia risk
- Fiber intake correlates with better lung function
Allergic Airway Disease
The gut microbiome affects asthma and allergies:
- Early-life dysbiosis increases allergy risk
- Beneficial bacteria promote tolerance
- Short-chain fatty acids have protective effects
- Restoring gut health can improve allergic conditions
Signs of Weak Mucosal Immunity
You might have compromised mucosal immunity if you experience:
- Frequent upper respiratory infections
- Recurring sinus infections
- Chronic cough or bronchitis
- Frequent urinary tract infections
- Recurring vaginal yeast infections
- Mouth ulcers or oral thrush
- Frequent digestive infections
- Food allergies or sensitivities
Strategies to Strengthen Mucosal Immunity
Dietary Approaches
Fermented foods support mucosal immune cells:
- Yogurt and kefir
- Fermented vegetables
- Miso and tempeh
- Traditional fermented foods from various cultures
Fiber feeds beneficial bacteria:
- Diverse plant fibers
- Prebiotic-rich foods
- Resistant starch
- Whole grains
Key nutrients for mucosal health:
- Vitamin A: Essential for mucosal cell maintenance
- Vitamin D: Modulates mucosal immune responses
- Zinc: Critical for mucosal immunity
- Glutamine: Fuel for mucosal cells
Lifestyle Factors
Avoid mucosal damage:
- Don't smoke (devastating to respiratory mucosa)
- Limit alcohol (damages gut and oral mucosa)
- Stay hydrated (mucus requires adequate water)
- Breathe through your nose (filters and conditions air)
Support mucosal regeneration:
- Adequate sleep allows tissue repair
- Manage stress which impairs mucosal immunity
- Moderate exercise enhances immune function
- Avoid unnecessary antibiotics
Targeted Probiotic Strategies
For respiratory protection:
- Lactobacillus rhamnosus strains
- Bifidobacterium animalis
- Oral probiotics (S. salivarius K12)
For gut mucosal immunity:
- Lactobacillus plantarum
- Bifidobacterium longum
- Various Lactobacillus species
For urogenital health:
- Lactobacillus crispatus
- Lactobacillus rhamnosus
- Lactobacillus reuteri

The Oral Microbiome Connection
Don't neglect your oral microbiome:
- It's the gateway to respiratory mucosal immunity
- Oral dysbiosis is linked to respiratory infections
- Avoid antibacterial mouthwashes that kill beneficial bacteria
- Consider oral probiotics for chronic respiratory issues
- Oral health affects systemic immune function
Building Stronger Mucosal Defenses
Strengthening mucosal immunity through the microbiome involves:
- Supporting gut microbiome diversity as the foundation
- Including fermented foods for immune-supporting bacteria
- Maintaining healthy mucosal surfaces through proper nutrition and hydration
- Avoiding factors that damage mucosa like smoking and excessive alcohol
- Considering targeted probiotics for specific mucosal areas of concern
Most people notice reduced frequency of mucosal infections within 2-3 months of consistent microbiome-supporting practices. Building robust mucosal immunity is an ongoing investment that pays dividends in overall health and resilience.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume fermented foods to support mucosal immune cells
- Include vitamin A-rich foods for mucosal health
- Stay hydrated to maintain mucosal moisture
- Avoid smoking and excessive alcohol which damage mucosa
- Practice nasal breathing to support respiratory microbiome
- Include glutamine-rich foods for mucosal cell nutrition
References
- Brandtzaeg P. The mucosal immune system and its integration with the mammary glands. Journal of Pediatrics. 2010;156(2 Suppl):S8-15. doi:10.1016/j.jpeds.2009.11.014
- Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nature Reviews Immunology. 2004;4(6):478-485. doi:10.1038/nri1373
- Bunker JJ, Bendelac A. IgA Responses to Microbiota. Immunity. 2017;49(2):211-224. doi:10.1016/j.immuni.2018.08.011
- Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336(6086):1268-1273. doi:10.1126/science.1223490
- Budden KF, Gellatly SL, Wood DLA, et al.. Emerging pathogenic links between microbiota and the gut-lung axis. Nature Reviews Microbiology. 2017;15(1):55-63. doi:10.1038/nrmicro.2016.142
- Cerf-Bensussan N, Gaboriau-Routhiau V. The immune system and the gut microbiota: friends or foes?. Nature Reviews Immunology. 2010;10(10):735-744. doi:10.1038/nri2850
