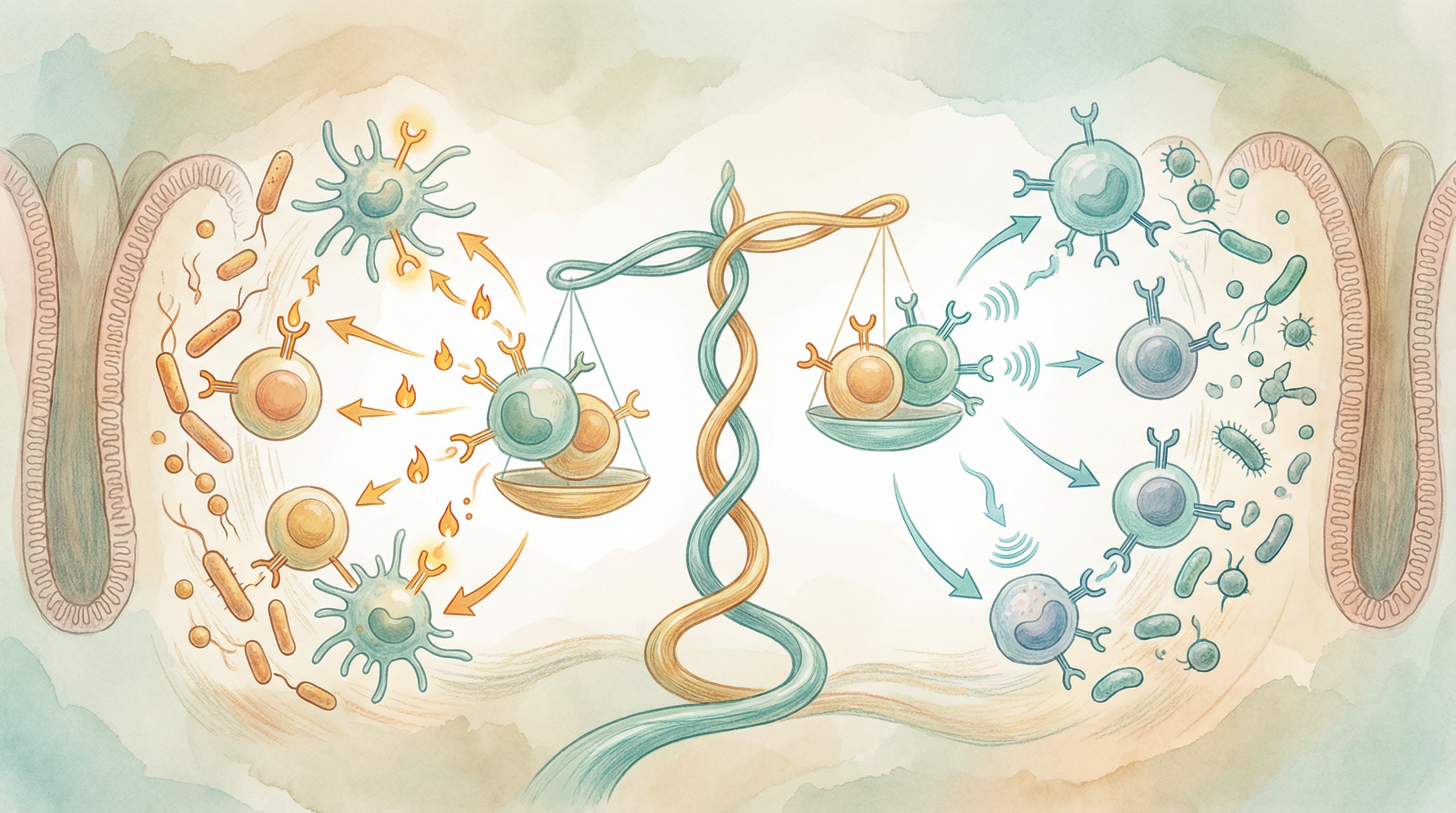
Balanced Inflammatory Response
Achieve optimal inflammation regulation through microbiome modulation, reducing chronic inflammation while maintaining effective acute responses.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Inflammation Balance
Inflammation is a double-edged sword. Acute inflammation is essential—it's how your body fights infections, heals wounds, and responds to threats. But chronic, low-grade inflammation underlies virtually every modern chronic disease, from heart disease and diabetes to autoimmune conditions and even depression[3].
Your gut microbiome is a master regulator of this balance, capable of either promoting or suppressing inflammation depending on its composition. Learning to cultivate an anti-inflammatory microbiome is one of the most powerful health interventions available.
How the Microbiome Regulates Inflammation
Short-Chain Fatty Acid Production
When beneficial bacteria ferment fiber, they produce SCFAs with powerful anti-inflammatory effects[1]:
Butyrate:
- Primary fuel for colon cells, maintaining barrier health
- Inhibits NF-κB, a master inflammatory switch
- Promotes regulatory T cell development
- Reduces inflammatory cytokine production
Propionate:
- Supports immune cell function
- Has anti-inflammatory effects in the colon
- May influence inflammation systemically through the liver
Acetate:
- Most abundant SCFA
- Contributes to overall immune regulation
- Supports beneficial bacterial growth
Regulatory T Cell Induction
Certain bacteria specifically promote immune tolerance:
- Bacteroides fragilis produces polysaccharide A (PSA), which activates regulatory T cells[2]
- These Tregs suppress excessive inflammatory responses
- They help maintain tolerance to food and self-antigens
- Their deficiency is associated with autoimmune conditions
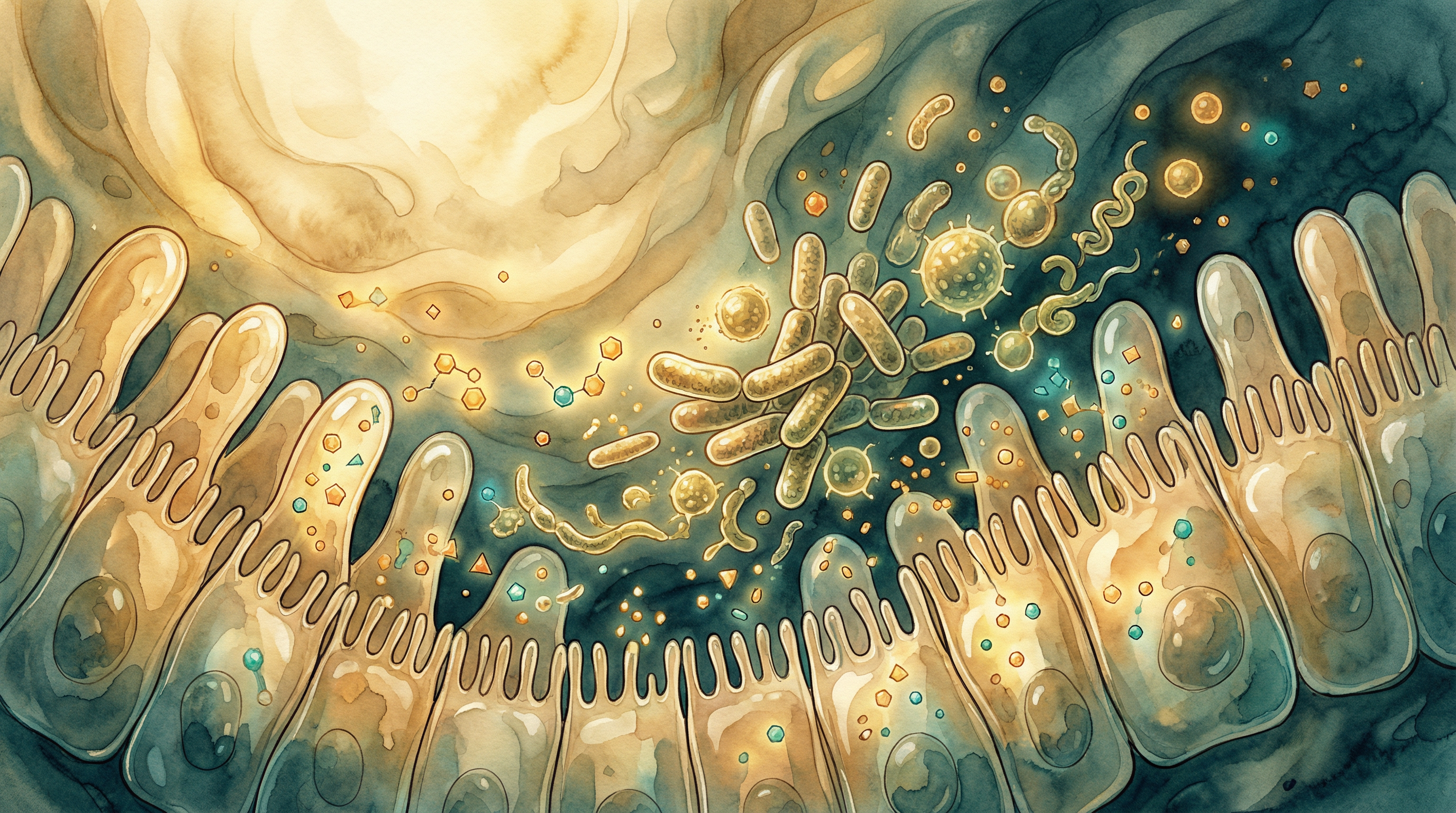
Barrier Integrity Maintenance
A healthy microbiome prevents inflammation by maintaining barriers. Research has shown that both Akkermansia muciniphila and Faecalibacterium prausnitzii play crucial roles in maintaining gut barrier integrity and reducing systemic inflammation[4]:
- Intact barriers prevent bacterial products from entering circulation
- Lipopolysaccharide (LPS) leakage triggers systemic inflammation
- This "metabolic endotoxemia" contributes to obesity-related inflammation
- Supporting barrier function is inherently anti-inflammatory
Immune Cell Programming
The microbiome shapes how immune cells behave:
- Determines the balance between pro- and anti-inflammatory cell types
- Influences the magnitude of immune responses
- Affects whether responses are appropriate or excessive
- Can help prevent autoimmune attack on self-tissues
Key Anti-Inflammatory Microbes
Faecalibacterium prausnitzii
Often called the most anti-inflammatory bacterium known[1]:
- Produces significant butyrate
- Secretes specific anti-inflammatory proteins
- Is depleted in inflammatory bowel disease
- Lower levels associated with many chronic conditions
- Responds well to prebiotic fiber intake
Akkermansia muciniphila
Critical for metabolic and immune health[5]:
- Maintains mucus layer integrity
- Associated with lower systemic inflammation
- Reduced in obesity, diabetes, and metabolic syndrome
- Produces proteins that improve barrier function
- Responds to polyphenol-rich foods
Studies have demonstrated that these two keystone species are consistently depleted in immune-related disorders, including autoimmune conditions and chronic inflammatory states[4].
Bacteroides fragilis
A master immune modulator[2]:
- Produces PSA that induces regulatory T cells
- Actively suppresses inflammatory responses
- Can protect against experimental colitis
- Represents how commensals actively promote health
Bacteroidales species also recruit specialized immune cells that promote barrier integrity in the colon[6].
Roseburia Species
Major butyrate producers:
- Ferment dietary fiber to produce anti-inflammatory SCFAs
- Support regulatory T cell development
- Often depleted in inflammatory conditions
- Thrive on resistant starch and fiber
The Inflammation-Disease Connection
Chronic low-grade inflammation contributes to:
Metabolic conditions:
- Type 2 diabetes
- Obesity
- Non-alcoholic fatty liver disease
- Metabolic syndrome
Cardiovascular disease:
- Atherosclerosis
- Hypertension
- Heart failure
Autoimmune conditions:
- Inflammatory bowel disease
- Rheumatoid arthritis
- Multiple sclerosis
- Psoriasis
Neurological conditions:
- Depression and anxiety
- Cognitive decline
- Neurodegenerative diseases
Other conditions:
- Certain cancers
- Chronic pain conditions
- Allergies and asthma
Signs of Inflammatory Imbalance
Chronic inflammation often manifests as:
- Persistent fatigue
- Body aches and joint pain
- Digestive problems
- Skin issues (acne, eczema, psoriasis)
- Mood disturbances
- Frequent infections
- Slow wound healing
- Weight gain, especially abdominal
- Brain fog
Dietary Strategies for Inflammation Balance
Anti-Inflammatory Foods
Omega-3 fatty acids:
- Fatty fish (salmon, mackerel, sardines)
- Walnuts and flaxseeds
- Chia seeds
- Algae supplements
Polyphenol-rich foods:
- Berries (especially blueberries)
- Green tea
- Dark chocolate
- Extra virgin olive oil
- Colorful vegetables
Fiber-rich foods for SCFA production:
- Legumes
- Whole grains
- Vegetables
- Fruits
- Nuts and seeds
Anti-inflammatory spices:
- Turmeric (with black pepper for absorption)
- Ginger
- Garlic
- Rosemary
Pro-Inflammatory Foods to Limit
Refined carbohydrates:
- White bread and pasta
- Pastries and baked goods
- Sugary cereals
Added sugars:
- Sodas and sweet drinks
- Candy and desserts
- Hidden sugars in processed foods
Processed meats:
- Bacon and sausage
- Deli meats
- Hot dogs
Industrial seed oils:
- Soybean oil
- Corn oil
- Cottonseed oil
Excessive alcohol:
- Damages gut barrier
- Promotes inflammatory bacteria
- Impairs immune function

Lifestyle Factors
Stress Management
Chronic stress is profoundly pro-inflammatory:
- Elevates cortisol, which affects microbiome composition
- Increases intestinal permeability
- Shifts immune responses toward inflammation
- Regular meditation, yoga, or breathing practices help
Sleep Quality
Poor sleep drives inflammation:
- Sleep deprivation increases inflammatory markers
- Disrupts microbiome circadian rhythms
- Impairs immune regulation
- Aim for 7-9 hours of quality sleep
Exercise
Moderate exercise is anti-inflammatory:
- Produces anti-inflammatory myokines
- Improves microbiome diversity
- Enhances immune regulation
- Excessive exercise without recovery can increase inflammation
Environmental Factors
Consider your toxic load:
- Air pollution increases inflammation
- Pesticide exposure may affect the microbiome
- Household chemicals can be pro-inflammatory
- Choose cleaner products when possible
Testing Inflammatory Status
Common markers include:
- High-sensitivity CRP (hs-CRP): General inflammation marker
- ESR (erythrocyte sedimentation rate): Another general marker
- Fasting insulin: Can indicate metabolic inflammation
- Ferritin: Elevated in inflammation
- Microbiome testing: Can identify anti-inflammatory species abundance
Building an Anti-Inflammatory Microbiome
The process typically involves:
- Reducing inflammatory triggers in diet and lifestyle
- Increasing fiber diversity to feed anti-inflammatory bacteria
- Including fermented foods for beneficial species
- Supporting barrier health to prevent LPS leakage
- Managing stress and sleep for optimal immune function
- Being patient — reducing chronic inflammation takes time
Most people notice improvements in inflammation-related symptoms within 4-8 weeks, though fully rebalancing the inflammatory system can take 3-6 months or longer for chronic conditions.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume omega-3 rich foods like fatty fish and walnuts
- Include turmeric and ginger with black pepper for absorption
- Eat colorful fruits and vegetables rich in polyphenols
- Limit refined sugars and processed foods
- Manage stress through regular meditation or mindfulness
- Prioritize quality sleep for immune regulation
References
- Sokol H, Pigneur B, Watterlot L, et al.. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium. Proceedings of the National Academy of Sciences. 2008;105(43):16731-16736. doi:10.1073/pnas.0804812105
- Mazmanian SK, Round JL, Kasper DL. A microbial symbiosis factor prevents intestinal inflammatory disease. Nature. 2008;453(7195):620-625. doi:10.1038/nature07008
- Tilg H, Moschen AR. Microbiota and diabetes: an evolving relationship. Gut. 2014;63(9):1513-1521. doi:10.1136/gutjnl-2014-306928
- Zhang T, Li P, Wu X, et al.. Akkermansia muciniphila and Faecalibacterium prausnitzii in immune-related diseases. Frontiers in Immunology. 2022;13:1089600. doi:10.3389/fimmu.2022.1089600
- Cani PD, de Vos WM. Next-generation beneficial microbes: the case of Akkermansia muciniphila. Frontiers in Microbiology. 2017;8:1765. doi:10.3389/fmicb.2017.01765
- Kuhn KA, Schulz HM, Regner EH, et al.. Bacteroidales recruit IL-6-producing intraepithelial lymphocytes in the colon to promote barrier integrity. Mucosal Immunology. 2018;11(2):357-368. doi:10.1038/mi.2017.55
