Enhanced Pathogen Defense
Strengthen your body's natural defenses against harmful bacteria, viruses, and fungi through a well-balanced gut microbiome.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
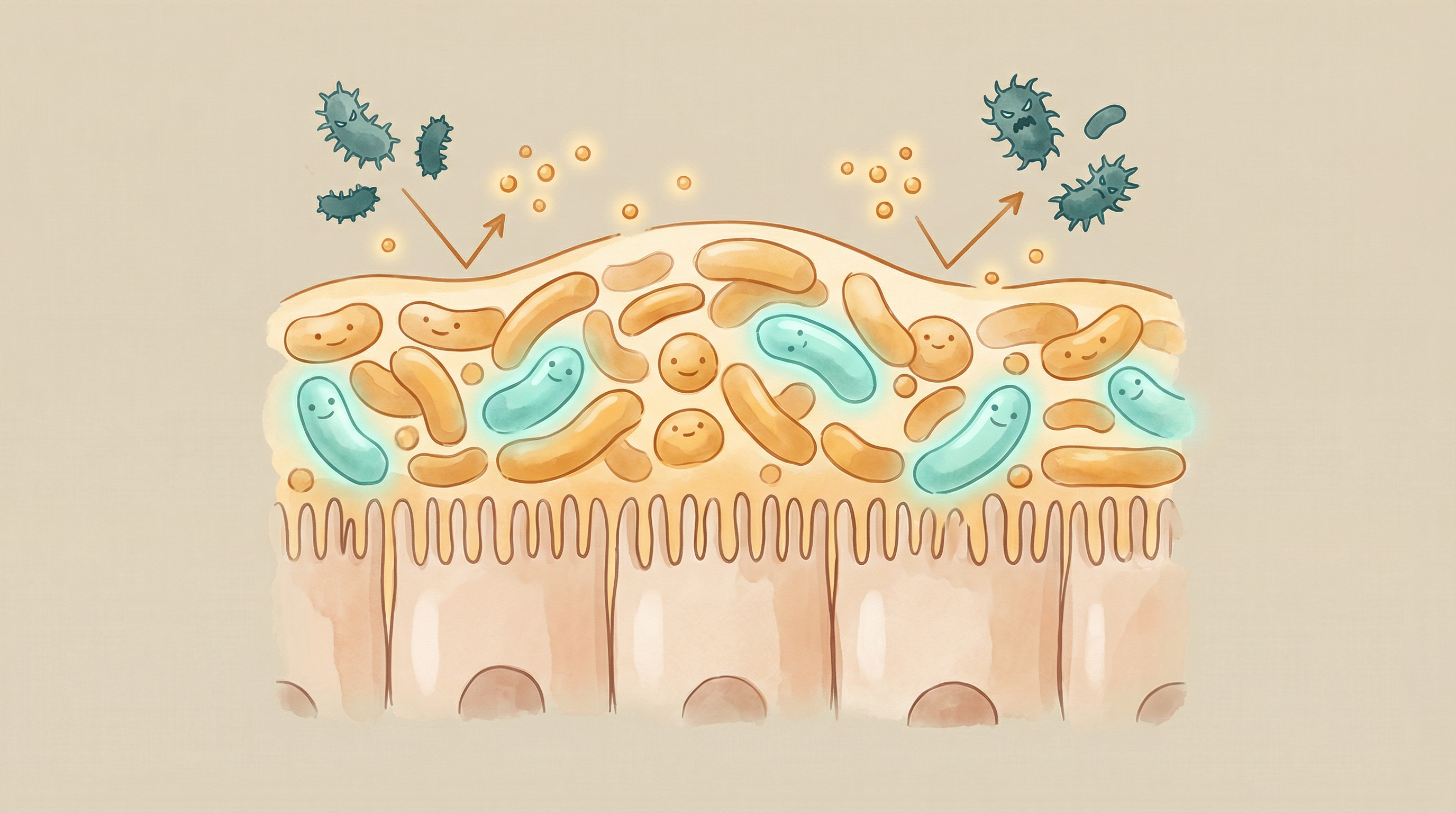
Your First Line of Defense
Before any invading pathogen can cause disease, it must first overcome an incredibly sophisticated defense system—your gut microbiome. The trillions of beneficial bacteria residing in your intestines form a living shield, employing multiple strategies to prevent harmful organisms from gaining a foothold[1].
This phenomenon, known as colonization resistance, is one of the most important and underappreciated aspects of immune function. A healthy, diverse microbiome can mean the difference between exposure to a pathogen and actual infection.
The Mechanisms of Colonization Resistance
Competitive Exclusion
Your beneficial bacteria physically occupy space and consume nutrients that pathogens would need[2]:
Physical blocking:
- Beneficial bacteria form dense communities on the gut lining
- They occupy attachment sites that pathogens would use
- This prevents pathogenic adhesion to intestinal cells
- A "lawn" of beneficial bacteria acts as a living barrier
Nutrient competition:
- Resident bacteria consume available sugars and amino acids
- This starves potential pathogens
- Complex carbohydrate fermenters particularly effective
- Iron sequestration is an important defense mechanism
Direct Antimicrobial Production
Many beneficial bacteria produce substances that directly kill or inhibit pathogens[4]:
Bacteriocins:
- Small antimicrobial peptides produced by bacteria
- Highly specific against related species
- Lactobacillus and Bifidobacterium produce many types
- Effective against Clostridium difficile and other pathogens
Organic acids:
- Lactic acid and acetic acid lower gut pH
- Most pathogens cannot survive in acidic environments
- SCFA production creates unfavorable conditions for pathogens
- Maintains a protective acidic microenvironment
Hydrogen peroxide:
- Produced by some Lactobacillus species
- Directly toxic to many pathogens
- Particularly important in vaginal health
- Creates an oxidative stress barrier
Bile Acid Modification
Gut bacteria modify bile acids in ways that affect pathogen survival:
- Secondary bile acids are more antimicrobial than primary ones
- Certain bile acids inhibit Clostridium difficile germination
- Microbiome disruption alters bile acid profiles
- Restoring normal bile acid patterns is part of recovery
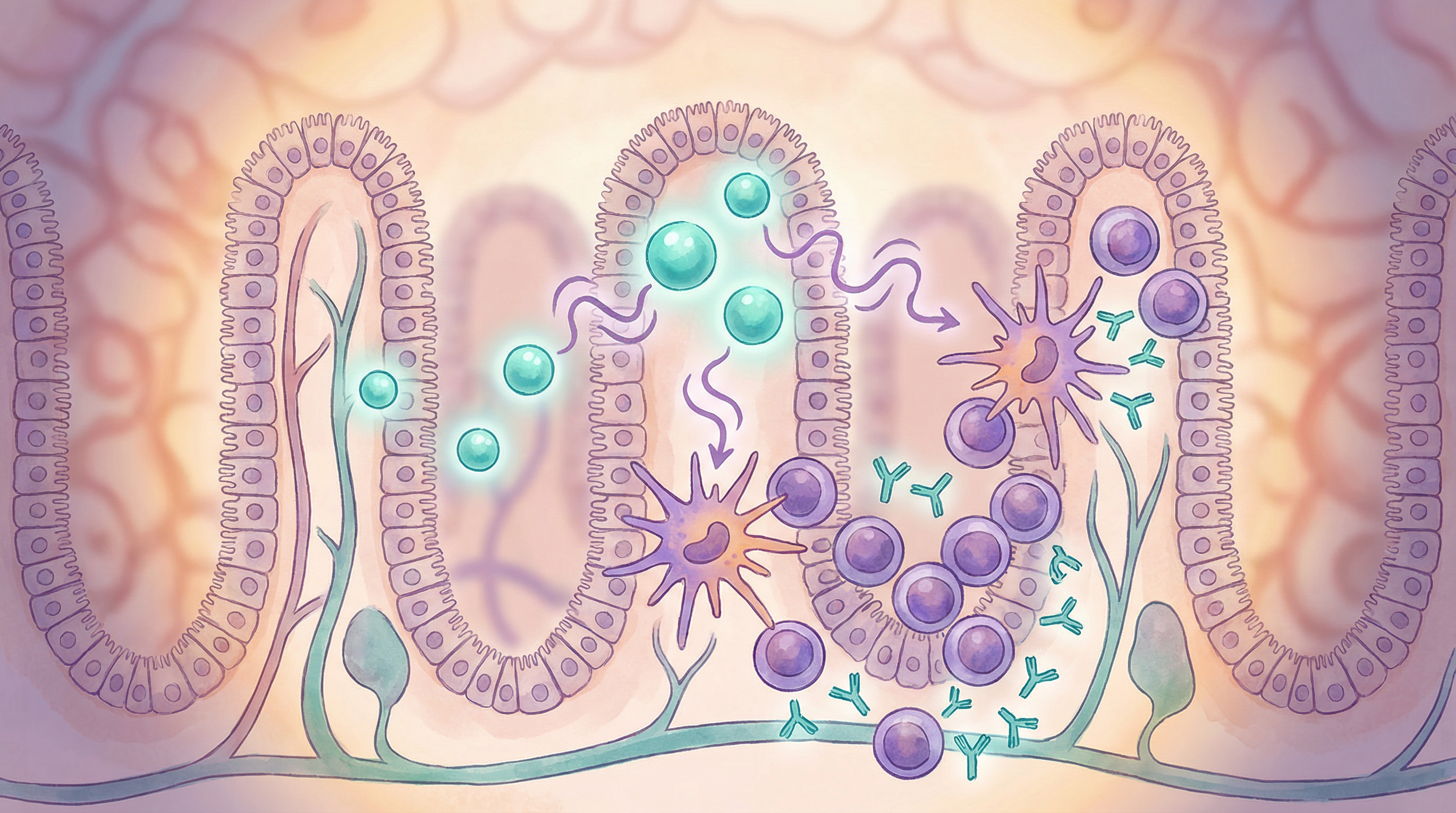
Immune System Training
The microbiome constantly educates and activates the immune system[3]:
- Keeps immune cells in a "ready" state
- Produces signals that enhance immune responses
- Trains the immune system to recognize dangerous patterns
- Promotes production of antimicrobial peptides by host cells
Key Defensive Species
Lactobacillus Species
Frontline defenders:
- Produce lactic acid, bacteriocins, and hydrogen peroxide
- Compete effectively for nutrients and attachment sites
- Enhance mucus production
- Support overall immune readiness
Bifidobacterium Species
Foundational protective bacteria[1]:
- Produce acetate and other inhibitory compounds
- Lower gut pH through fermentation
- Support the growth of other beneficial species
- Important in early life pathogen resistance
Bacteroides thetaiotaomicron
A key sentinel species:
- Trains the immune system to respond appropriately
- Produces antimicrobial compounds
- Signals to host cells to produce defensins
- Maintains barrier function
Akkermansia muciniphila
Mucus layer guardian:
- Maintains healthy mucus thickness
- Supports barrier integrity
- Associated with reduced pathogen translocation
- Responds to polyphenol-rich foods
Clinical Evidence for Colonization Resistance
Research has demonstrated the profound importance of microbiome-mediated pathogen defense[6]:
Antibiotic-Associated Infections
Studies show that antibiotics disrupt colonization resistance:
- Disruption of normal microbiome allows pathogen expansion
- Clostridium difficile infection is a classic example
- Risk correlates with degree of microbiome disruption
- Recovery of resistance requires microbiome restoration
Pathogen-Specific Protection
Specific microbiome members protect against specific pathogens:
- Bacteroides species protect against Salmonella
- Clostridium scindens protects against C. difficile
- Diverse communities provide broader protection
- Loss of key species creates vulnerabilities
Fecal Microbiota Transplantation
The ultimate proof of colonization resistance:
- FMT restores pathogen defense in C. difficile patients
- Success rates exceed 90% for recurrent infection
- Demonstrates causality of microbiome in protection
- Specific protective consortia being identified
Signs of Weakened Pathogen Defense
You may have compromised colonization resistance if you experience:
- Frequent gastrointestinal infections
- Recurrent foodborne illnesses
- Susceptibility to traveler's diarrhea
- History of C. difficile infection
- Frequent urinary tract infections
- Recurring vaginal infections
- Increased illness frequency after antibiotic use
Building Stronger Pathogen Defense
Dietary Strategies
Diverse fiber intake:
- Feeds the full range of protective bacteria
- Promotes SCFA production and acidification
- Supports barrier function
- Enhances competitive exclusion
Fermented foods:
- Introduce beneficial Lactobacillus species
- Provide organic acids directly
- Support overall microbiome diversity
- Traditional ferments may be particularly beneficial
Prebiotic foods:
- Garlic, onions, leeks (allium vegetables)
- Asparagus, Jerusalem artichokes
- Bananas, especially slightly green
- Oats and barley
Polyphenol-rich foods:
- Support Akkermansia and other protective species
- Berries, green tea, dark chocolate
- Extra virgin olive oil
- Red wine (moderate amounts)
Lifestyle Factors
Antibiotic stewardship:
- Use antibiotics only when truly necessary
- Complete prescribed courses when used
- Support recovery with diet and possibly probiotics
- Discuss alternatives with healthcare providers
Stress management:
- Chronic stress impairs gut barrier
- Reduces beneficial bacterial populations
- Increases susceptibility to infection
- Regular relaxation practices help
Sleep quality:
- Sleep deprivation weakens immune function
- Disrupts microbiome composition
- Impairs barrier function
- Prioritize consistent, quality sleep
Targeted Support
Probiotics:
- Lactobacillus and Bifidobacterium strains
- May be particularly helpful after antibiotics
- Look for strains with research support
- Consider timing around antibiotic doses
Prebiotics:
- Feed existing beneficial bacteria
- Support SCFA production
- Can enhance probiotic effectiveness
- Gradually increase intake

Protecting Colonization Resistance
To maintain strong pathogen defense:
- Preserve microbiome diversity through varied diet
- Support barrier function with fiber and polyphenols
- Minimize unnecessary disruptions like excessive antibiotics
- Actively rebuild after necessary microbiome disturbances
- Maintain overall immune health through sleep and stress management
- Consider targeted probiotics during high-risk periods
Colonization resistance is a gift from millions of years of co-evolution between humans and our microbial partners. By supporting and maintaining this living defense system, we tap into one of nature's most sophisticated protection mechanisms.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume diverse fermented foods to introduce beneficial bacteria
- Eat prebiotic-rich foods like garlic, onions, and asparagus
- Avoid unnecessary antibiotic use
- Stay hydrated to support mucus barrier function
- Get adequate vitamin D through sunlight or supplementation
- Include zinc-rich foods like pumpkin seeds and legumes
References
- Buffie CG, Pamer EG. Microbiota-mediated colonization resistance against intestinal pathogens. Nature Reviews Immunology. 2013;13(11):790-801. doi:10.1038/nri3535
- Kamada N, Chen GY, Inohara N, Núñez G. Control of pathogens and pathobionts by the gut microbiota. Nature Immunology. 2013;14(7):685-690. doi:10.1038/ni.2608
- Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121-141. doi:10.1016/j.cell.2014.03.011
- Lawley TD, Walker AW. Intestinal colonization resistance. Immunology. 2013;138(1):1-11. doi:10.1111/j.1365-2567.2012.03616.x
- Vollaard EJ, Clasener HAL. Colonization resistance. Antimicrobial Agents and Chemotherapy. 1994;38(3):409-414. doi:10.1128/AAC.38.3.409
- Ducarmon QR, Zwittink RD, Hornung BVH, et al.. Gut microbiota and colonization resistance against bacterial enteric infection. Microbiology and Molecular Biology Reviews. 2019;83(3):e00007-19. doi:10.1128/MMBR.00007-19
