Enhanced Gut-Brain Signaling
Optimize the bidirectional communication between your gut and brain through microbiome support for improved mood, cognition, and stress response.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Two-Way Conversation
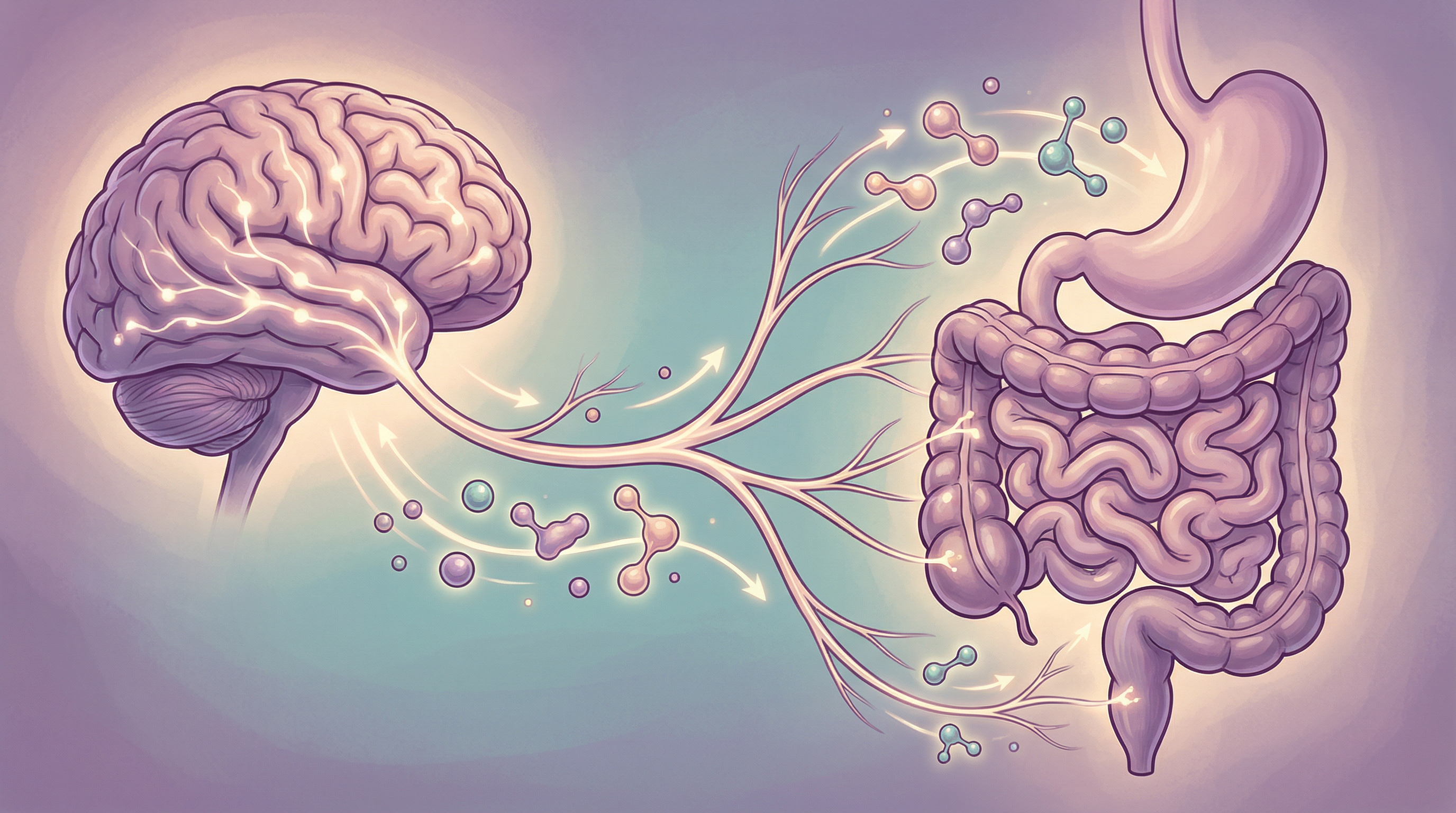
Your gut and brain are in constant communication through a complex network known as the gut-brain axis. This isn't a one-way street—information flows continuously in both directions, with your brain affecting gut function and your gut profoundly influencing your mental state[3].
At the center of this communication network sits your gut microbiome, acting as a critical mediator that can either enhance or disrupt gut-brain signaling. Optimizing this communication is fundamental to mental health and cognitive performance.
The Communication Highways
The Vagus Nerve: The Main Connection
The vagus nerve is the primary neural pathway between gut and brain[2]:
Anatomy:
- Longest cranial nerve in the body
- 80% of its fibers carry signals from gut to brain (afferent)
- 20% carry signals from brain to gut (efferent)
- Directly connects gut bacteria to brain function
Functions:
- Monitors gut environment and conveys status to brain
- Regulates heart rate and breathing
- Controls digestive processes
- Influences mood and stress response
Bacterial influence:
- Certain bacteria activate vagal afferents
- This triggers changes in brain function[1]
- Cutting the vagus nerve blocks many probiotic effects
- Vagal tone correlates with mental health
The Immune Pathway
Immune signaling connects gut inflammation to brain function:
- Cytokines produced in the gut reach the brain
- Immune cells activated in the gut can enter the brain
- Gut inflammation triggers brain immune responses
- Anti-inflammatory bacteria reduce neuroinflammation
The Metabolite Highway
Bacterial metabolites travel via circulation. A comprehensive review in Physiological Reviews characterized this as a complex signaling network involving multiple pathways[4]:
Short-chain fatty acids:
- Cross the blood-brain barrier
- Directly affect brain cells
- Influence neurotransmitter production
- Modulate neuroinflammation
Tryptophan metabolites:
- Affect serotonin availability
- Some are neuroprotective, others neurotoxic
- Balance depends on microbiome composition
Other neuroactive compounds:
- GABA, dopamine precursors
- Histamine
- Various other signaling molecules
The Hormonal System
The hypothalamic-pituitary-adrenal (HPA) axis:
- Regulates stress response
- Is influenced by gut bacteria
- Affects mood and cognition
- Can be dysregulated by dysbiosis
How Bacteria Influence the Brain
Direct Neurotransmitter Production
Gut bacteria produce neuroactive compounds[5]:
- Serotonin (mostly made in the gut)
- GABA (calming neurotransmitter)
- Dopamine precursors
- Norepinephrine
Vagal Activation
Certain bacteria specifically activate the vagus nerve[1]:
- Lactobacillus rhamnosus changes brain GABA receptors via the vagus
- Bifidobacterium longum reduces stress response through vagal signaling
- These effects disappear if the vagus nerve is cut
Barrier Regulation
Healthy gut-brain signaling requires intact barriers:
- Gut barrier prevents inflammatory leakage
- Blood-brain barrier protects the brain
- Both are influenced by microbiome composition
Immune Modulation
By shaping immune function, bacteria affect brain signaling:
- Anti-inflammatory bacteria reduce brain inflammation
- Pro-inflammatory species increase it
- Balanced immunity supports clear signaling

Signs of Impaired Gut-Brain Communication
You might have disrupted gut-brain signaling if you experience:
- Mood swings unrelated to obvious causes
- Gut symptoms that worsen with stress
- Brain fog or mental clarity issues
- Anxiety or depression with gut involvement
- Stress that triggers digestive upset
- Difficulty with emotional regulation
- Poor stress tolerance
- Fatigue despite adequate sleep
Key Psychobiotic Species
Research on psychobiotics—bacteria that produce mental health benefits—has identified several key species[6]:
Lactobacillus rhamnosus
The most researched psychobiotic:
- Directly activates vagal pathways
- Changes GABA receptor expression in the brain
- Reduces anxiety and depression-like behaviors
- Strain JB-1 particularly well-studied
Bifidobacterium longum
Powerful stress-response modulator:
- Reduces HPA axis activation
- Improves cognitive performance under stress
- Lowers cortisol levels
- Strain 1714 shows anxiolytic effects
Lactobacillus helveticus
Often combined with B. longum:
- Reduces anxiety and depression measures
- Improves sleep quality
- Combination R0052/R0175 is well-researched
- Enhances overall gut-brain communication
Roseburia Species
Important for metabolite signaling:
- Major butyrate producers
- SCFAs directly affect brain function
- Support overall gut-brain axis health
- Respond well to dietary fiber
Strategies to Enhance Gut-Brain Signaling
Vagus Nerve Activation
Deep breathing:
- Slow, diaphragmatic breathing activates the vagus
- Practice 5-10 minutes daily
- Box breathing or 4-7-8 technique
Cold exposure:
- Cold showers or face immersion
- Activates vagal response
- Start gradually
Singing, humming, gargling:
- Activate vagal motor fibers
- Simple and accessible
- Practice regularly
Meditation:
- Increases vagal tone
- Improves gut-brain communication
- Multiple techniques effective
Dietary Support
Fermented foods:
- Introduce psychobiotic species
- Support overall microbiome health
- Include variety (yogurt, kefir, sauerkraut, miso)
Fiber for SCFA production:
- Diverse plant fibers
- Resistant starch
- Prebiotic-rich foods
Omega-3 fatty acids:
- Support neuronal membrane health
- Have anti-inflammatory effects
- May enhance vagal function
Polyphenols:
- Feed beneficial bacteria
- Have direct neuroprotective effects
- Include berries, green tea, dark chocolate
Lifestyle Factors
Exercise:
- Enhances vagal tone
- Improves microbiome diversity
- Reduces stress hormones
- Boosts brain-derived neurotrophic factor
Sleep:
- Essential for gut-brain axis function
- Supports microbiome circadian rhythms
- Allows neural restoration
Stress management:
- Chronic stress impairs gut-brain communication
- Mind-body practices restore balance
- Social connection is protective
Nature exposure:
- Contact with nature reduces stress
- May diversify the microbiome
- Improves overall well-being
Testing Gut-Brain Function
Assessment options include:
- Heart rate variability: Measures vagal tone
- Cortisol testing: Shows HPA axis function
- Microbiome testing: Reveals psychobiotic abundance
- Inflammatory markers: Indicate gut-brain inflammation
- Neurotransmitter metabolites: Show production patterns

Building Better Communication
Enhancing gut-brain signaling through the microbiome involves:
- Supporting psychobiotic species through diet and potentially supplements
- Activating the vagus nerve through breathing, cold exposure, and other practices
- Reducing inflammation that disrupts signaling
- Managing stress which impairs gut-brain communication
- Maintaining healthy barriers to ensure clean signal transmission
Most people notice improvements in mood, stress response, and mental clarity within 4-8 weeks of consistent gut-brain supporting practices. Optimizing this complex communication network is an ongoing process that deepens over months of sustained effort.
Supporting Practices
Evidence-based strategies to support this benefit:
- Practice deep breathing exercises to stimulate the vagus nerve
- Include fermented foods to support psychobiotic bacteria
- Engage in regular physical activity
- Practice mindfulness meditation
- Cold exposure (cold showers) to enhance vagal tone
- Humming or singing to activate the vagus nerve
References
- Bravo JA, Forsythe P, Chew MV, et al.. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences. 2011;108(38):16050-16055. doi:10.1073/pnas.1102999108
- Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience. 2018;12:49. doi:10.3389/fnins.2018.00049
- Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Journal of Clinical Investigation. 2015;125(3):926-938. doi:10.1172/JCI76304
- Cryan JF, O'Riordan KJ, Cowan CSM, et al.. The Microbiota-Gut-Brain Axis. Physiological Reviews. 2019;99(4):1877-2013. doi:10.1152/physrev.00018.2018
- Dinan TG, Cryan JF. Gut instincts: microbiota as a key regulator of brain development, ageing, and neurodegeneration. The Journal of Physiology. 2017;595(2):489-503. doi:10.1113/JP273106
- Sarkar A, Lehto SM, Harty S, et al.. Psychobiotics and the Manipulation of Bacteria-Gut-Brain Signals. Trends in Neurosciences. 2016;39(11):763-781. doi:10.1016/j.tins.2016.09.002
