Reduced Neuroinflammation
Decrease brain inflammation through microbiome modulation to protect cognitive function, improve mood, and reduce risk of neurodegenerative conditions.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
The Silent Threat: Brain Inflammation
Neuroinflammation—inflammation in the brain and central nervous system—is increasingly recognized as a driver of mental health disorders, cognitive decline, and neurodegenerative diseases. Unlike inflammation elsewhere in the body, brain inflammation often goes unnoticed until it causes significant damage[1].
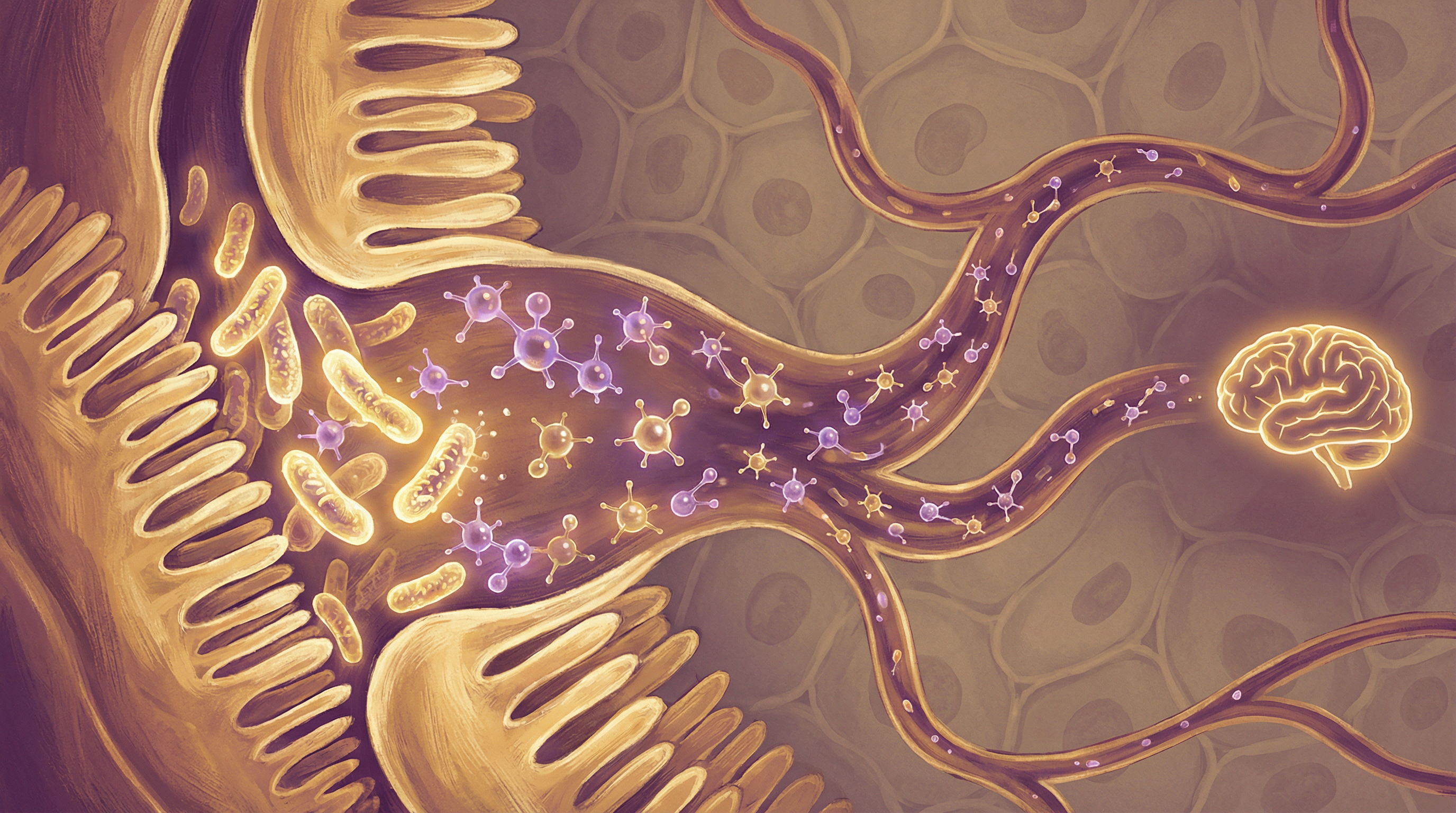
What makes this particularly relevant is the discovery that your gut microbiome has profound influence over brain inflammation. The gut-brain axis doesn't just affect mood—it shapes the inflammatory state of your entire nervous system.
How the Microbiome Influences Brain Inflammation
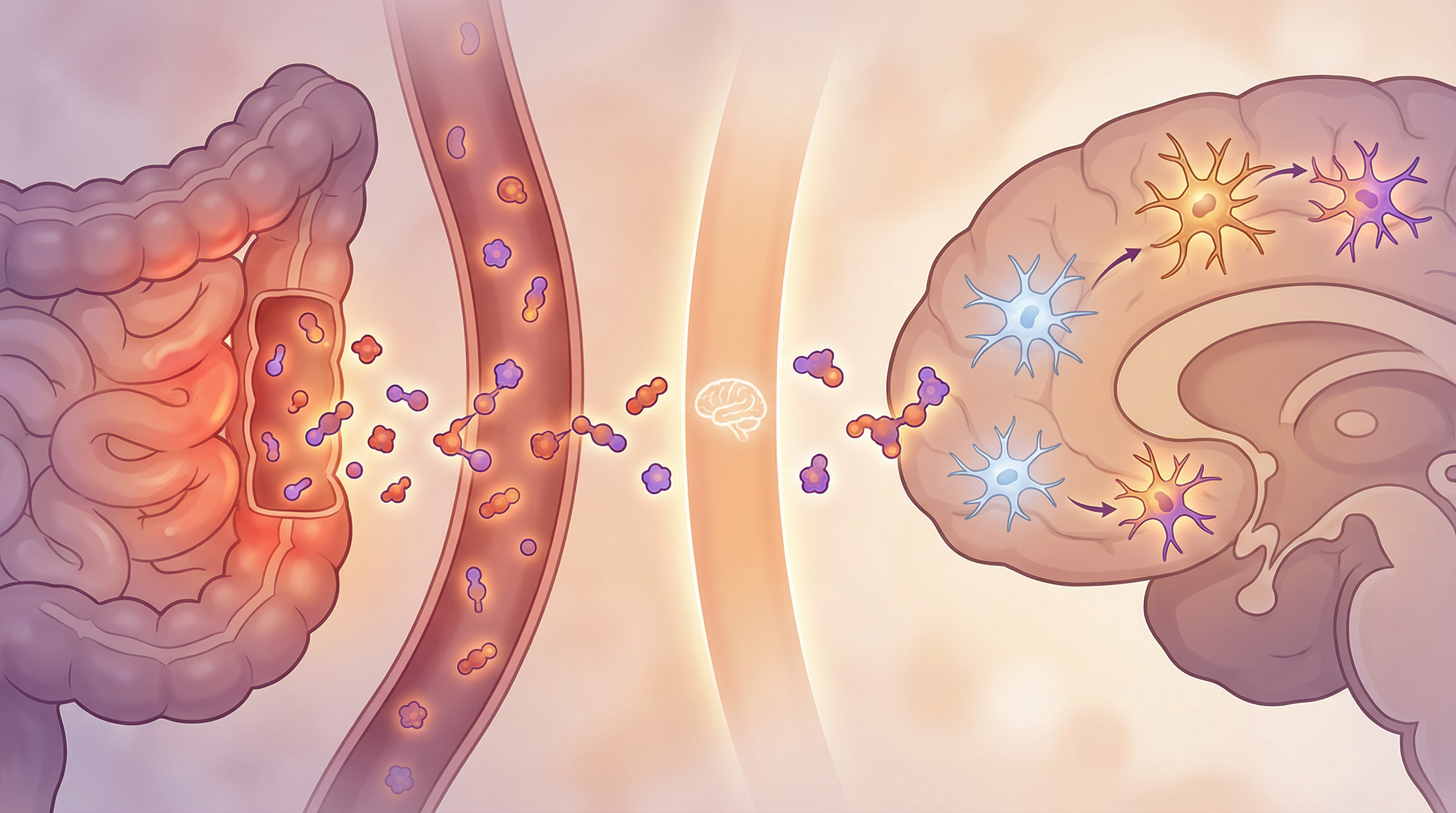
The Gut-Brain Inflammatory Pathway
Multiple mechanisms connect gut bacteria to brain inflammation:
Vagus nerve signaling:
- The vagus nerve directly connects gut and brain
- Inflammatory signals from gut dysbiosis travel this route
- Anti-inflammatory signals from beneficial bacteria do too
- Vagal tone affects both gut and brain inflammation
Systemic inflammation:
- Gut dysbiosis increases intestinal permeability
- Bacterial products (like LPS) enter circulation
- These trigger systemic inflammatory responses
- Inflammatory molecules cross the blood-brain barrier
Metabolite effects:
- Short-chain fatty acids from beneficial bacteria reduce brain inflammation
- Tryptophan metabolites can be neuroprotective or neurotoxic
- Other bacterial metabolites directly affect brain immune cells
Microglia: The Brain's Immune Cells
Microglia are the primary immune cells of the brain[3]. Recent research has shown that the microbiome influences microglia in a sex-specific manner, affecting brain development throughout life[6]:
Normal functions:
- Monitor brain environment for threats
- Clear debris and dead cells
- Support synaptic pruning and plasticity
- Maintain brain homeostasis
Microbiome dependence:
- Germ-free animals have abnormal microglia
- Microglia require microbiome-derived signals to mature
- Dysbiosis leads to dysregulated microglial activation
- Chronic microglial activation drives neuroinflammation
When things go wrong:
- Overactive microglia produce inflammatory molecules
- This damages neurons and disrupts function
- Chronic activation is seen in depression, anxiety, and neurodegeneration
- Supporting the microbiome can help restore balance
The Blood-Brain Barrier
This protective barrier separates brain from blood:
- Gut inflammation can increase barrier permeability
- A "leaky brain" allows inflammatory substances to enter
- Certain gut bacteria help maintain barrier integrity
- SCFAs from beneficial bacteria strengthen the barrier
Conditions Linked to Neuroinflammation
Mental Health Disorders
Depression:
- Elevated inflammatory markers common in depression
- Anti-inflammatory treatments can improve symptoms
- Microbiome-targeting approaches show promise
Anxiety:
- Neuroinflammation affects anxiety circuitry
- Gut inflammation exacerbates anxiety
- Anti-inflammatory bacteria reduce anxiety in studies
Brain fog:
- Inflammation impairs cognitive processing
- Often accompanies gut dysfunction
- Responds to anti-inflammatory interventions
Neurodegenerative Diseases
Parkinson's disease:
- Alpha-synuclein pathology may start in the gut[2]
- Gut inflammation precedes brain pathology
- Microbiome composition affects disease progression
Alzheimer's disease:
- Neuroinflammation is a key disease feature
- Gut dysbiosis correlates with amyloid deposition[5]
- Germ-free mice show reduced amyloid pathology[4]
- Targeting gut bacteria may slow progression
Multiple sclerosis:
- Autoimmune attack on myelin involves inflammation
- Gut bacteria influence immune tolerance
- Microbiome interventions being explored
Key Anti-Inflammatory Microbes
Faecalibacterium prausnitzii
The most potent anti-inflammatory gut bacterium:
- Produces significant butyrate
- Secretes specific anti-inflammatory proteins
- Depleted in many inflammatory conditions
- Supports microglial health through SCFA production
Akkermansia muciniphila
Critical for barrier integrity:
- Maintains mucus layer health
- Reduces systemic inflammation
- Associated with better metabolic health
- May help prevent inflammatory signals reaching the brain
Bifidobacterium longum
Well-studied for brain-gut effects:
- Reduces inflammatory cytokines
- Improves stress response
- Strain 1714 specifically reduces neuroinflammation
- Supports overall gut-brain axis health
Lactobacillus plantarum
Versatile anti-inflammatory species:
- Produces various anti-inflammatory compounds
- Supports gut barrier function
- Reduces anxiety and depression markers
- May directly influence brain inflammation
Signs of Neuroinflammation
Consider neuroinflammation if you experience:
- Brain fog or difficulty concentrating
- Memory problems
- Mood disturbances (depression, anxiety)
- Fatigue that doesn't improve with rest
- Headaches
- Sensitivity to light or sound
- Sleep disturbances
- Declining cognitive function
Dietary Strategies to Reduce Brain Inflammation
Anti-Inflammatory Foods
Omega-3 fatty acids:
- Fatty fish (salmon, mackerel, sardines)
- Algae-based supplements for vegetarians
- Walnuts and flaxseeds
- Target EPA and DHA specifically
Polyphenol-rich foods:
- Blueberries (particularly neuroprotective)
- Dark chocolate
- Green tea
- Extra virgin olive oil
- Colorful fruits and vegetables
Anti-inflammatory spices:
- Turmeric (with black pepper for absorption)
- Ginger
- Rosemary
- Cinnamon
Fiber for SCFA production:
- Diverse plant fibers
- Resistant starch
- Legumes
- Whole grains
Pro-Inflammatory Foods to Limit
Refined sugars:
- Spike inflammation
- Feed inflammatory bacteria
- Disrupt blood sugar regulation
Processed foods:
- Contain inflammatory additives
- Often high in omega-6 fatty acids
- Low in protective nutrients
Excessive alcohol:
- Directly neurotoxic
- Increases gut permeability
- Disrupts microbiome
Industrial seed oils:
- High omega-6 content
- May promote inflammation
- Prefer olive oil and other traditional fats

Lifestyle Factors for Brain Health
Sleep
Critical for clearing brain inflammation:
- Glymphatic system clears inflammatory debris during sleep
- Sleep deprivation increases neuroinflammatory markers
- Aim for 7-9 hours of quality sleep
- Maintain consistent sleep schedule
Exercise
Physical activity reduces brain inflammation:
- Produces anti-inflammatory myokines
- Increases blood-brain barrier integrity
- Supports microbiome diversity
- Enhances glymphatic clearance
Stress Management
Chronic stress is profoundly pro-inflammatory:
- Activates microglia
- Disrupts the gut-brain axis
- Increases inflammatory cytokines
- Regular meditation measurably reduces brain inflammation
Cognitive Engagement
Mental stimulation is neuroprotective:
- Supports synaptic health
- May reduce inflammatory processes
- Learning new skills is particularly beneficial
- Social engagement also protective
Testing and Assessment
Markers that may indicate neuroinflammation:
- High-sensitivity CRP: General inflammation marker
- Inflammatory cytokines: IL-6, TNF-alpha, IL-1beta
- Microbiome testing: Can reveal dysbiosis patterns
- Organic acids testing: Shows metabolite imbalances
- Cognitive testing: Baseline and follow-up assessments
Building a Neuroprotective Microbiome
Reducing neuroinflammation through the microbiome involves:
- Increasing anti-inflammatory bacteria through diet and lifestyle
- Reducing gut permeability to prevent inflammatory signals
- Boosting SCFA production through fiber intake
- Minimizing inflammatory triggers in diet and environment
- Supporting overall gut-brain axis health through comprehensive approaches
Most people notice improvements in brain fog and mood within 4-8 weeks of consistent anti-inflammatory practices. Reducing established neuroinflammation and its effects typically requires 3-6 months or longer of sustained effort, but the cognitive and mental health benefits are substantial.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume omega-3 fatty acids from fatty fish or algae
- Include turmeric with black pepper for curcumin absorption
- Eat polyphenol-rich berries, especially blueberries
- Limit refined sugars and processed foods
- Practice regular meditation or mindfulness
- Ensure adequate quality sleep
References
- Cryan JF, O'Riordan KJ, Cowan CSM, et al.. The Microbiota-Gut-Brain Axis. Physiological Reviews. 2019;99(4):1877-2013. doi:10.1152/physrev.00018.2018
- Sampson TR, Debelius JW, Thron T, et al.. Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson's Disease. Cell. 2016;167(6):1469-1480. doi:10.1016/j.cell.2016.11.018
- Erny D, Hrabě de Angelis AL, Kipnis J, et al.. Host microbiota constantly control maturation and function of microglia in the CNS. Nature Neuroscience. 2015;18(7):965-977. doi:10.1038/nn.4030
- Harach T, Marungruang N, Duthilleul N, et al.. Reduction of Abeta amyloid pathology in APPPS1 transgenic mice in the absence of gut microbiota. Scientific Reports. 2017;7:41802. doi:10.1038/srep41802
- Vogt NM, Kerby RL, Dill-McFarland KA, et al.. Gut microbiome alterations in Alzheimer's disease. Scientific Reports. 2017;7(1):13537. doi:10.1038/s41598-017-13601-y
- Thion MS, Low D, Silvin A, et al.. Microbiome Influences Prenatal and Adult Microglia in a Sex-Specific Manner. Cell. 2018;172(3):500-516. doi:10.1016/j.cell.2017.11.042