Gardnerella vaginalis is the primary initiating pathogen in bacterial vaginosis (BV), acting as a scaffold organism for polymicrobial biofilm formation[1]. Recent reclassification has identified 13 distinct genomic species within the Gardnerella genus, with varying pathogenic potential and antibiotic resistance profiles[2]. BV affects approximately 25% of pregnant women globally and is associated with a 3.4-fold increased risk of chlamydia and 4.1-fold increased risk of gonorrhea acquisition.
Key Characteristics
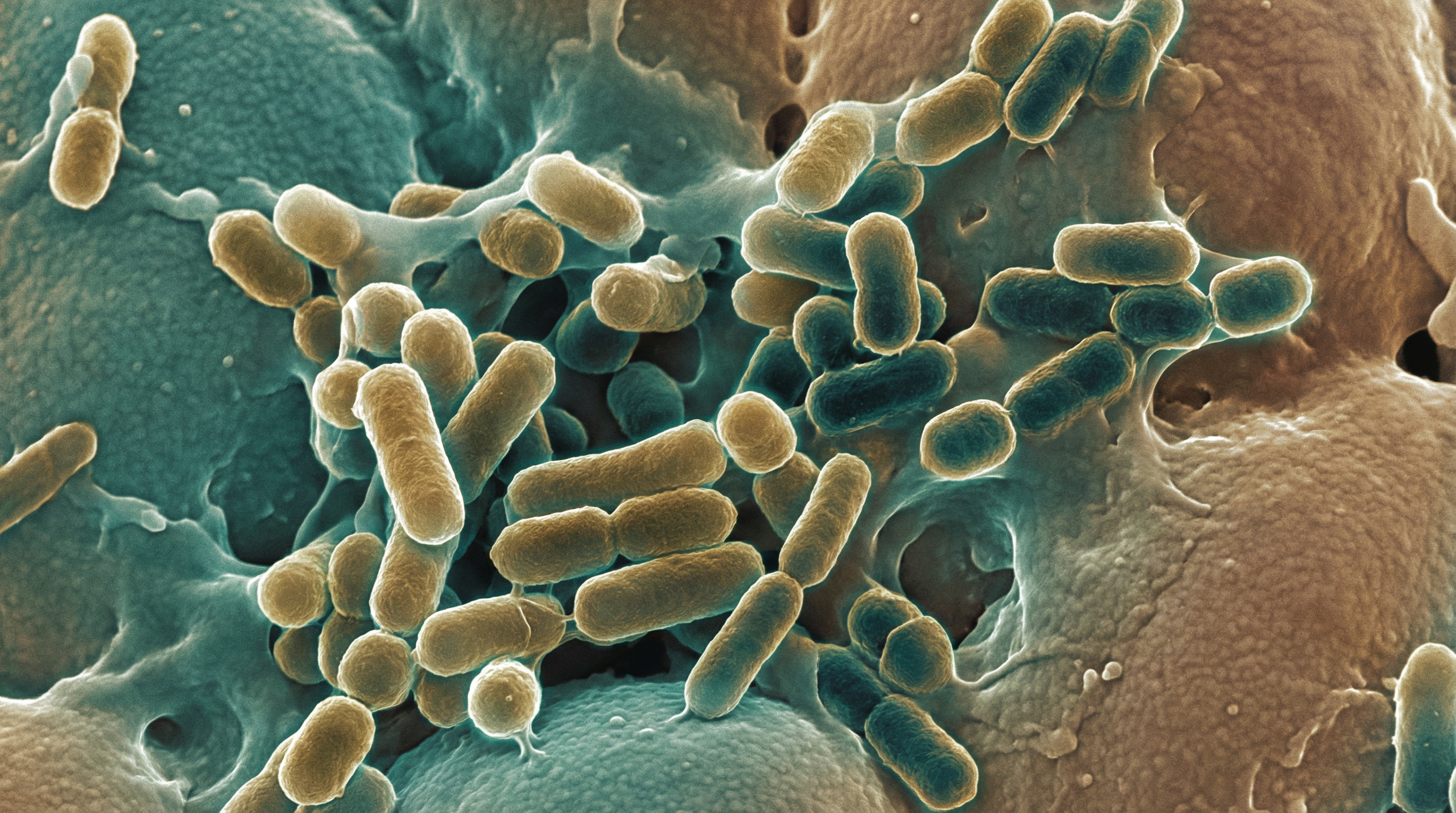
G. vaginalis is a pleomorphic rod-shaped, facultatively anaerobic bacterium with sophisticated virulence mechanisms. The organism has been reclassified from a single species into 13 genomic species including G. vaginalis (Clade 1), G. piotii (Clade 2), G. leopoldii and G. swidsinskii (Clade 4), and Subgroup D (Clade 3). Clades 1 and 3 are most strongly associated with symptomatic BV, while species diversity explains why colonization does not always result in clinical disease[3]. The bacterium colonizes 95-100% of BV cases but is also present in 97% of healthy women at significantly lower bacterial loads.
Virulence Factors
Vaginolysin (VLY)
Vaginolysin is a cholesterol-dependent pore-forming cytolysin (CDC) that is human-specific, binding CD59 complement regulatory molecules on human cells[4]. Genetic knockout studies in 2025 definitively proved VLY as the primary driver of Gardnerella cytotoxicity—VLY-deficient mutants showed zero hemolytic activity and no LDH release in human cervical tissue explants, while wild-type caused significant damage within 12-24 hours. VLY exists in multiple types (1A, 1B, 1C, 2, 3) with Type 1A showing highest cytotoxicity. Beyond direct tissue damage, VLY lyses neutrophils as an immune evasion tactic and liberates intracellular sugars (CMP-Neu5Ac) that Neisseria gonorrhoeae scavenges for complement evasion.
Sialidases (NanH1, NanH2, NanH3)
G. vaginalis produces three sialidase enzymes that cleave terminal sialic acids from host glycoproteins[5]:
- NanH1 (Sialidase A): Primary enzyme for host vaginal mucus degradation; nanH1-deficient mutants showed significant reduction in competitive fitness and persistence in murine models
- NanH2: Extracellular sialidase that degrades cervical mucus and remodels sperm glycocalyx
- NanH3: Essential for human cervical mucus degradation
A groundbreaking 2024 study demonstrated that Gardnerella sialidases directly impair sperm function—desialylation reduces sperm surface charge, increases agglutination, and triggers complement-mediated immobilization, establishing a mechanistic link between BV and infertility[6]. These effects were reversed by sialidase inhibitors (DANA, ZANA) and C3 inhibitors.
Biofilm Formation and Sexual Transmission
G. vaginalis acts as the scaffold organism for multi-species BV biofilms through a four-stage process[7]:
- Initial adhesion (0-4h): Attachment via fimbriae, serine-rich-repeat lectins, and Cna proteins
- Microcolony formation (4-24h): Bacterial proliferation and EPS production; formation of "clue cells"
- Biofilm maturation (24-48h): Multi-species development with Autoinducer-2 (AI-2) quorum sensing; hypoxic microenvironment supporting obligate anaerobes (Prevotella, Atopobium vaginae, Mobiluncus)
- Dispersion (48h+): Release of planktonic bacteria; biofilm persistence causing treatment failure
The landmark StepUp Trial published in NEJM (2025) demonstrated that BV is sexually transmitted—treating male partners with oral metronidazole plus topical clindamycin cream reduced BV recurrence from 63% to 35% (HR 0.37, 95% CI 0.22-0.61)[8]. Men harbor BV species in the distal urethra and subpreputial space, and penile microbiota composition is highly predictive of a woman's BV risk.
Antibiotic Resistance
Resistance patterns vary dramatically by Gardnerella clade:
- Clades 3 and 4: 100% metronidazole resistance
- Clade 1: 35% resistance
- Mechanisms: nim genes (nitroreductases), McrA endonucleases, ABC transporters (YadH), biofilm protection, pH-dependent ion trapping reducing drug uptake, iron scavenging decreasing metronidazole activation
These resistance patterns explain the 50-70% recurrence rates within 3-6 months following standard antibiotic treatment.
Pregnancy and STI Implications
BV affects approximately 25% of pregnant women globally (range 4.9-49%), with highest prevalence in African populations[9]. Maternal outcomes include:
- Preterm birth: Via bacterial ascension triggering intrauterine inflammation
- Chorioamnionitis: Found in 55.6% of BV cases
- Premature rupture of membranes: Through enzymatic membrane weakening
- Spontaneous abortion: From early pregnancy infection
Fetal/neonatal outcomes include low birth weight, NICU admission, respiratory distress, neonatal sepsis, and long-term neurocognitive delays. BV significantly increases STI acquisition risk—HIV (enhanced by NLRP3 inflammasome activation and increased CD4+ T cells), chlamydia (3.4-fold; BV bacteria produce indole allowing Chlamydia to bypass IFN-γ tryptophan starvation), and gonorrhea (4.1-fold; VLY liberates sialic acids for gonococcal complement evasion).
Emerging Therapeutics
Endolysin Therapy (BNT331)
A first-in-human Phase 1/2 trial (NCT06469164) initiated July 2024 is testing BNT331-endolysin vaginal inserts[10]. Preclinical data showed:
- 94% reduction in viable Gardnerella load over 19 hours
- 99.7-99.8% growth inhibition at 20-500 μg/mL
- Lactobacillus crispatus remained viable and proliferated
- Narrow-spectrum targeting sparing beneficial microbiota
Other Novel Approaches
- LACTIN-V: Live Lactobacillus crispatus CTV-05 biotherapeutic significantly reduces BV recurrence
- Vaginal microbiome transplantation: Transfer of healthy donor vaginal secretions for refractory cases
- Sialidase inhibitors: DANA and ZANA block enzyme activity, preventing mucus degradation
- Anti-biofilm agents: Boric acid, lactic acid gels, DNase (degrades eDNA matrix)
Microbiome Interactions
G. vaginalis exhibits the highest virulence among BV-associated bacteria, characterized by superior initial adhesion, cytotoxic effects, and biofilm-forming capacity. Key interactions include:
- GBS synergy: S. agalactiae senses Gardnerella density via quorum sensing, producing AI-2 at 0.76 nM to 7.6 µM that significantly increases biofilm thickness
- Lactobacillus displacement: High ability to displace protective L. crispatus from epithelial cells; L. iners (less protective) fails to prevent pathogen overgrowth
- UTI facilitation: Gardnerella induces urothelial exfoliation and IL-1R-mediated inflammation, triggering emergence of uropathogenic E. coli from intracellular reservoirs
- Chlamydia support: BV bacteria produce indole allowing C. trachomatis to bypass host tryptophan starvation
