Bacteroides fragilis
Bacteroides fragilis is a Gram-negative, obligate anaerobic, non-spore-forming, rod-shaped bacterium belonging to the phylum Bacteroidetes. It is a prominent member of the human gut microbiota with a complex and multifaceted relationship with its host. B. fragilis exhibits a remarkable duality, functioning both as a beneficial commensal organism and as an opportunistic pathogen when displaced from its normal intestinal habitat.
Key Characteristics
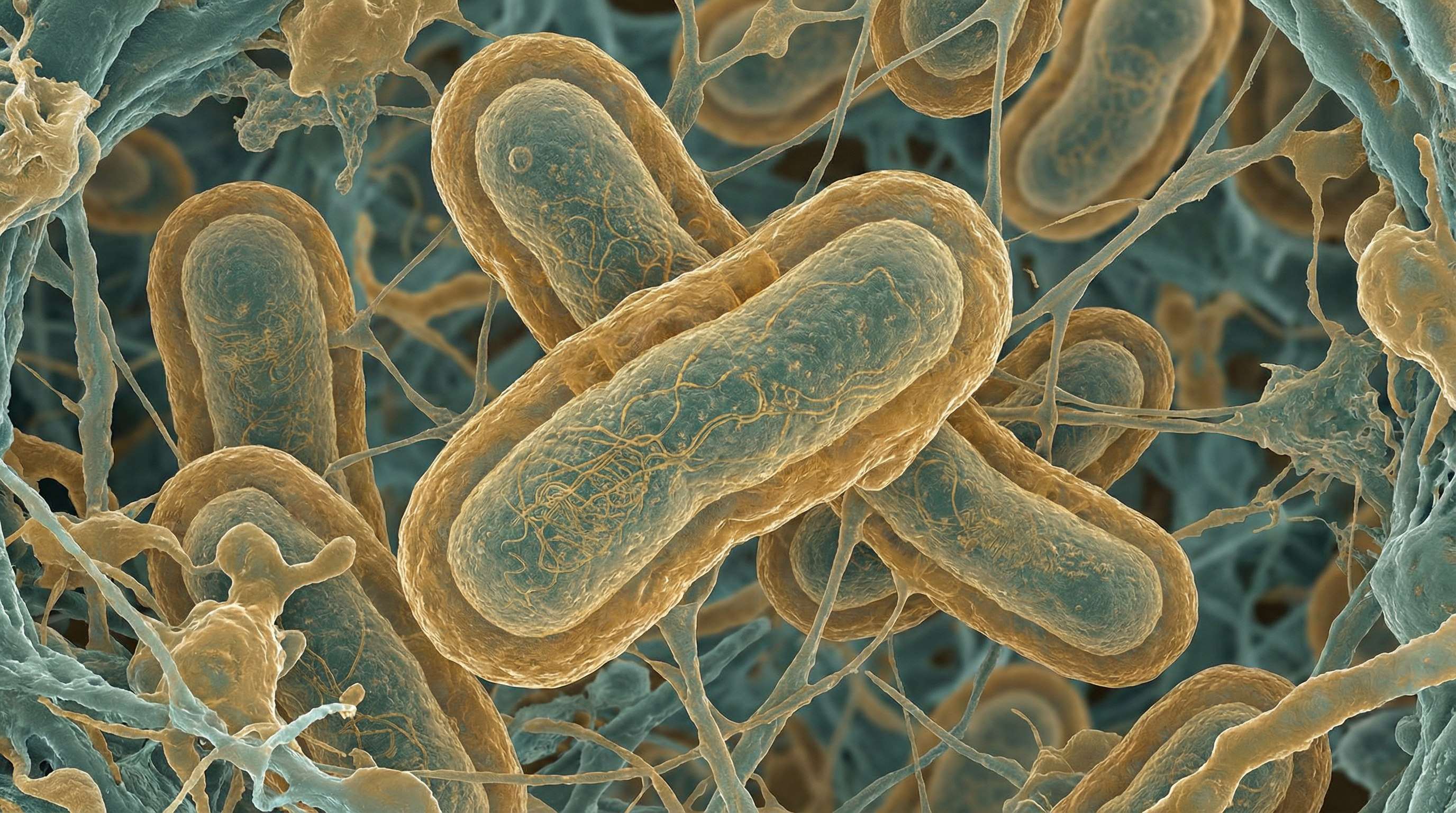
B. fragilis is characterized by its pleomorphic rod shape and its status as an obligate anaerobe, meaning it cannot survive in the presence of oxygen. It is non-motile and encapsulated, with the capsule playing a crucial role in its interactions with the host immune system. A distinctive feature of B. fragilis is its genetic commitment to capsular polysaccharide synthesis, with the ability to produce eight different capsular polysaccharides (designated A-H)—an extraordinary number compared to most bacteria, which typically produce only one if any.
The bacterium possesses a complex cell surface structure with numerous outer membrane proteins and lipopolysaccharides that contribute to its virulence and immunomodulatory properties. B. fragilis is also notable for its resistance to many antibiotics, including penicillins, due to the production of beta-lactamase enzymes.
Among the capsular polysaccharides, polysaccharide A (PSA) has been extensively studied for its unique immunomodulatory properties. Unlike most bacterial polysaccharides, PSA possesses zwitterionic characteristics, carrying both positive and negative charges on the same repeating sugar molecule. This unusual property allows PSA to be processed by antigen-presenting cells and activate T cells in a protein-like manner, making it a powerful modulator of the host immune system.
Role in the Human Microbiome
B. fragilis primarily inhabits the human colon, where it constitutes approximately 0.5-1% of the gut microbiota. Despite its relatively low abundance compared to other Bacteroides species, it plays disproportionately important roles in host health and disease through its metabolic activities and interactions with the immune system.
In the gut microbiome, B. fragilis contributes to:
Maintenance of intestinal homeostasis: Through the production of PSA, B. fragilis helps regulate the balance between pro-inflammatory and anti-inflammatory immune responses in the gut.
Colonization resistance: It competes with potential pathogens for nutrients and ecological niches, helping to prevent colonization by harmful bacteria.
Metabolism of complex carbohydrates: B. fragilis possesses an extensive array of glycoside hydrolases and polysaccharide lyases that enable it to break down complex dietary and host-derived glycans that other bacteria cannot digest.
Production of short-chain fatty acids (SCFAs): Through fermentation, it generates beneficial metabolites that serve as energy sources for colonocytes and regulate immune responses.
Development and maturation of the immune system: PSA from B. fragilis has been shown to correct Th1/Th2 cytokine imbalances and promote the development of regulatory T cells.
The ecological niche of B. fragilis within the gut is primarily the mucus layer adjacent to the intestinal epithelium, where it can access host-derived glycans and interact closely with the mucosal immune system.
Health Implications
Beneficial Effects
B. fragilis, particularly through its PSA, has demonstrated several beneficial effects on host health:
Protection against inflammatory diseases: B. fragilis and PSA have been shown to protect against experimental colitis, encephalomyelitis, and asthma in animal models by promoting anti-inflammatory immune responses.
Immune system education: The bacterium plays a role in training the immune system to distinguish between harmful and beneficial microbes, contributing to immune tolerance.
Regulation of type I interferons: B. fragilis regulates basal levels of type I interferons, which are critical for antiviral immunity. Studies have shown that B. fragilis or PSA alone can increase interferon-β gene expression, enhancing protection against viral infections.
Colorectal cancer protection: Some studies suggest that B. fragilis may have protective effects against colorectal cancer development through its immunomodulatory properties.
Pulmonary inflammation reduction: B. fragilis has been shown to reduce pulmonary inflammation in animal models, suggesting potential benefits for respiratory health.
Detrimental Effects
Despite its beneficial roles, B. fragilis can cause significant harm under certain circumstances:
Opportunistic infections: When displaced outside the gut or when it escapes into the bloodstream following disruption of the mucosal surface (during surgery, trauma, or inflammation), B. fragilis can cause serious infections, including:
- Intra-abdominal abscesses
- Bacteremia and sepsis
- Soft tissue infections
- Brain abscesses
Enterotoxigenic strains: Some strains of B. fragilis produce a metalloprotease toxin called Bacteroides fragilis toxin (BFT), which can damage the intestinal epithelium, potentially contributing to inflammatory bowel disease and colorectal cancer.
Alzheimer's disease association: Recent research has identified a potential role for B. fragilis in Alzheimer's disease pathogenesis. Studies have shown that B. fragilis and its metabolites 12-hydroxy-heptadecatrienoic acid (12-HHTrE) and Prostaglandin E2 (PGE2) can activate microglia and induce Alzheimer's disease pathologies in susceptible mouse models.
Antibiotic resistance: B. fragilis exhibits resistance to multiple antibiotics, including penicillins and some cephalosporins, complicating treatment of infections.
The balance between beneficial and harmful effects of B. fragilis depends on factors such as its location in the body, the specific strain, host genetic factors, and the overall composition of the gut microbiota.
Metabolic Activities
B. fragilis possesses a versatile metabolism that enables it to thrive in the competitive environment of the human gut:
Carbohydrate metabolism: It can utilize a wide range of complex carbohydrates, including dietary fiber, host-derived glycans, and mucins. This metabolic flexibility is supported by an extensive repertoire of carbohydrate-active enzymes encoded in its genome.
Polysaccharide synthesis: A significant portion of the B. fragilis genome is dedicated to the synthesis of capsular polysaccharides, reflecting the importance of these structures for its survival and interactions with the host.
Short-chain fatty acid production: Through fermentation of carbohydrates, B. fragilis produces beneficial metabolites such as acetate, propionate, and succinate, which serve as energy sources for colonocytes and have immunomodulatory effects.
Bile acid metabolism: B. fragilis can metabolize primary bile acids, contributing to the pool of secondary bile acids in the gut, which influence host metabolism and immune function.
Polyunsaturated fatty acid (PUFA) metabolism: B. fragilis produces metabolites from PUFAs, including 12-HHTrE and PGE2, which have been implicated in neuroinflammation and Alzheimer's disease pathogenesis.
Protein metabolism: It possesses proteolytic enzymes that enable it to utilize dietary and host-derived proteins as nutrient sources.
Resistance mechanisms: B. fragilis has evolved various metabolic strategies to resist host defense mechanisms and antibiotics, including the production of beta-lactamases and efflux pumps.
These metabolic activities not only support the growth and survival of B. fragilis in the gut but also influence host physiology through the production of bioactive metabolites that can affect local and systemic immune responses.
Clinical Relevance
B. fragilis is clinically significant in several contexts:
Intra-abdominal infections: B. fragilis is one of the most common anaerobic bacteria isolated from intra-abdominal infections, including peritonitis and abscesses. These infections typically occur when the intestinal barrier is breached, allowing gut bacteria to enter the peritoneal cavity.
Bacteremia: Although less common than other types of bacteremia, B. fragilis bloodstream infections are associated with high mortality rates (approximately 19-45%) due to the bacterium's virulence factors and antibiotic resistance.
Antibiotic resistance: B. fragilis is resistant to penicillin due to beta-lactamase production. It also shows variable resistance to other antibiotics, including cefoxitin, moxifloxacin, and clindamycin. Metronidazole remains the antibiotic of choice for most B. fragilis infections, although resistance rates of 0.5-7.8% have been reported.
Polymicrobial infections: B. fragilis infections are typically polymicrobial, involving other anaerobes and facultative anaerobes. This polymicrobial nature complicates treatment and often requires broad-spectrum antibiotic coverage.
Emerging treatments: Newer antibiotics such as eravacycline (a novel fluorocycline) and tazobactam/ceftolozane in combination with metronidazole have shown promising activity against B. fragilis in clinical trials.
Potential therapeutic applications: Paradoxically, given its role as an opportunistic pathogen, purified PSA from B. fragilis is being investigated as a potential therapeutic agent for inflammatory conditions due to its immunomodulatory properties. There is interest in developing B. fragilis as a next-generation probiotic or engineering PSA into a carbohydrate-based vaccine.
Alzheimer's disease connection: The emerging link between B. fragilis and Alzheimer's disease suggests potential new therapeutic targets for this neurodegenerative condition, focusing on modulating the gut microbiota or neutralizing specific bacterial metabolites.
Management of B. fragilis infections requires a multidisciplinary approach involving infectious disease specialists, surgeons, radiologists, and clinical pharmacists to ensure appropriate antibiotic selection and adequate source control.
Interaction with Other Microorganisms
B. fragilis engages in complex interactions with other members of the gut microbiota and with potential pathogens:
Competitive interactions: B. fragilis competes with other gut bacteria for nutrients and ecological niches. This competition helps maintain microbial diversity and prevents the overgrowth of potential pathogens.
Cooperative interactions: It may engage in cross-feeding relationships with other gut bacteria, where metabolic byproducts from one species serve as substrates for another, contributing to the overall stability of the gut ecosystem.
Modulation of the gut microbiota composition: Through its production of antimicrobial compounds and competition for resources, B. fragilis can influence the overall composition of the gut microbiota.
Interactions with pathogens: B. fragilis can inhibit the growth of certain pathogens through direct competition or through stimulation of host immune responses. Conversely, disruption of the normal gut microbiota (e.g., by antibiotics) can allow for the expansion of enterotoxigenic B. fragilis strains.
Biofilm formation: B. fragilis can form biofilms, which facilitate interactions with other microorganisms and provide protection against environmental stressors, including antibiotics and host immune responses.
Horizontal gene transfer: B. fragilis can exchange genetic material with other bacteria through horizontal gene transfer, potentially acquiring virulence factors or antibiotic resistance genes.
Immune system modulation: Through PSA and other factors, B. fragilis can shape the host immune response in ways that affect interactions with other microorganisms, potentially promoting tolerance to beneficial commensals while enhancing responses against pathogens.
These interactions highlight the ecological importance of B. fragilis in the gut microbiome and its potential as both a contributor to health and a cause of disease, depending on the context and the specific strains involved.
In conclusion, Bacteroides fragilis represents a fascinating example of the complex relationships between gut bacteria and their human hosts. Its dual nature as both a beneficial commensal and an opportunistic pathogen, its unique immunomodulatory properties through PSA, and its emerging connections to conditions like Alzheimer's disease make it a subject of intense scientific interest. Understanding the factors that determine whether B. fragilis acts as a friend or foe in the gut microbiome may lead to new therapeutic approaches for a range of inflammatory, infectious, and neurodegenerative diseases.
