Papillomaviridae in the Human Virome
Overview
Papillomaviridae is a diverse family of small, non-enveloped, double-stranded DNA viruses that specifically infect epithelial cells of vertebrates in a species-specific manner. Human papillomaviruses (HPVs) represent a large group within this family, with over 200 distinct types identified to date. These viruses are ubiquitous in human populations and constitute a significant component of the human virome.
HPVs are characterized by their strict epitheliotropism, infecting basal cells of stratified epithelia in the skin and mucous membranes. Their life cycle is intimately linked to the differentiation program of the infected epithelial cells, with viral genome amplification, late gene expression, and virion assembly occurring in progressively differentiated epithelial layers. This unique replication strategy allows HPVs to establish persistent infections that can last for years or even decades.
The clinical significance of HPVs ranges from completely asymptomatic infections to benign proliferative lesions (warts) and malignant neoplasms. Based on their oncogenic potential, HPVs are classified into high-risk and low-risk types. High-risk HPVs, particularly types 16 and 18, are causally associated with cervical cancer and a proportion of other anogenital and oropharyngeal cancers. Low-risk types, such as HPV 6 and 11, primarily cause benign genital warts and rarely progress to malignancy.
Recent metagenomic studies have revealed that HPV infections are much more prevalent in healthy individuals than previously recognized, with different body sites harboring distinct HPV communities. This suggests that many HPV types may be commensal members of the human microbiome, with their pathogenic potential influenced by factors such as viral persistence, host immune status, and interactions with other microbiome components.
Characteristics
Virion Structure
Papillomaviruses have a characteristic structure that includes:
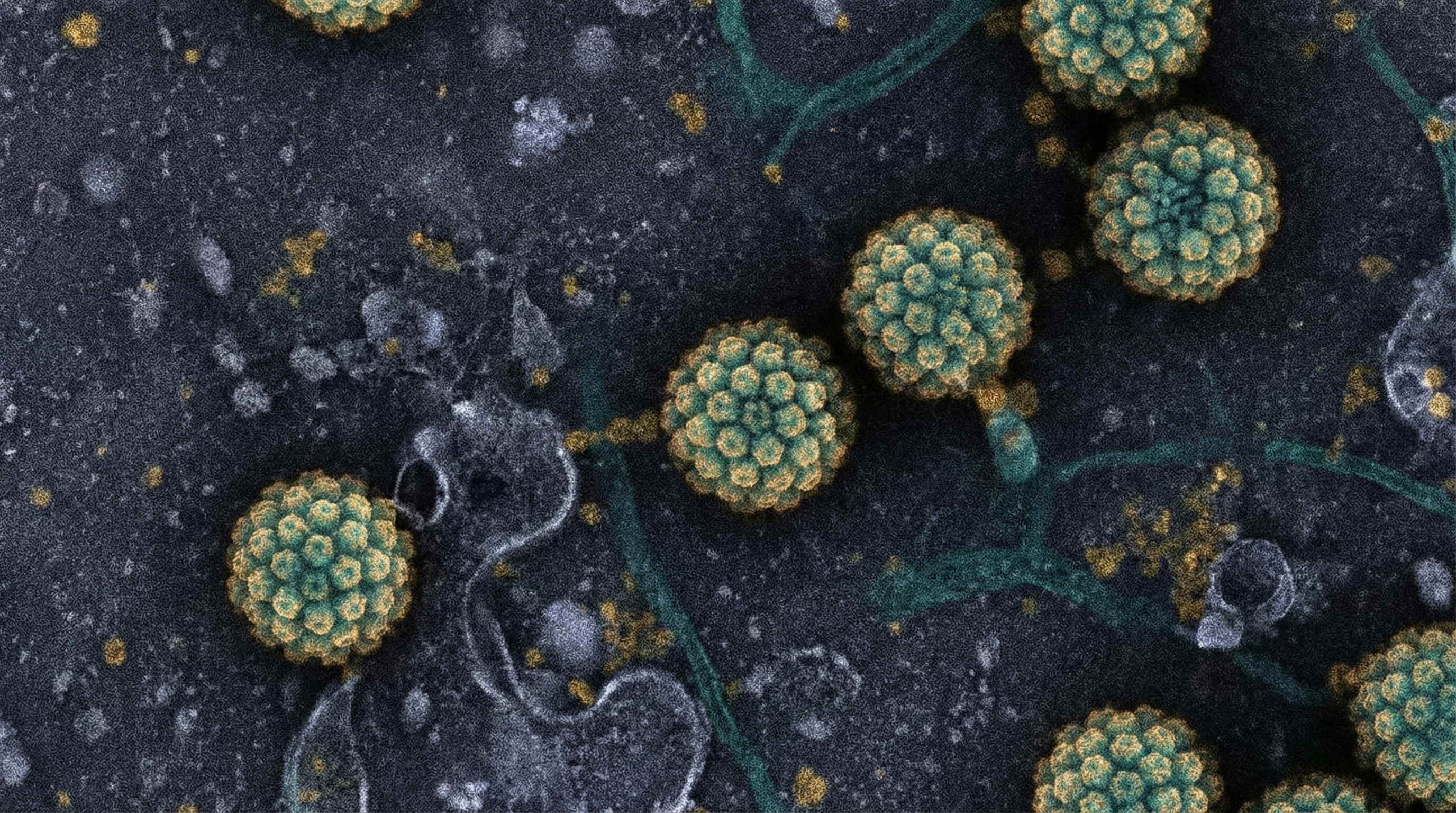
Capsid: A non-enveloped, icosahedral capsid approximately 55-60 nm in diameter, composed of 72 capsomeres (pentamers of the major capsid protein L1).
Genome: A circular, double-stranded DNA genome of approximately 8,000 base pairs, which is associated with cellular histones to form a chromatin-like complex within the virion.
Minor Capsid Protein: The L2 protein, present in smaller amounts than L1, is embedded within the capsid and plays crucial roles in infection and virion assembly.
Genomic Organization
The HPV genome is organized into three functional regions:
Early Region (E): Contains genes (E1-E7) that encode proteins necessary for viral replication and cellular transformation:
- E1: DNA helicase essential for viral replication
- E2: Regulates viral transcription and replication
- E4: Disrupts cytokeratin networks to facilitate virion release
- E5: Modulates cellular signaling pathways
- E6: Oncoprotein that targets p53 for degradation (in high-risk types)
- E7: Oncoprotein that binds and inactivates pRb (in high-risk types)
Late Region (L): Contains genes (L1-L2) that encode the structural capsid proteins:
- L1: Major capsid protein that self-assembles into virus-like particles
- L2: Minor capsid protein involved in virion assembly and infection
Long Control Region (LCR): A non-coding regulatory region containing the origin of replication and transcription factor binding sites that control viral gene expression.
Viral Life Cycle
The HPV life cycle is tightly linked to the differentiation program of the infected epithelium:
Infection: HPV infects basal epithelial cells, likely through microabrasions that expose the basement membrane. Initial attachment involves binding to heparan sulfate proteoglycans, followed by conformational changes in the capsid that facilitate entry.
Establishment: Following entry, the viral genome is transported to the nucleus, where it is maintained as a low-copy-number episome (circular extrachromosomal DNA). Early viral genes are expressed at low levels.
Maintenance: As infected basal cells divide, viral episomes are partitioned to daughter cells, maintaining the infection in the proliferating cell population.
Amplification: When infected cells enter the differentiation program and migrate upward in the epithelium, the viral genome is amplified to high copy numbers, and late genes are expressed.
Assembly and Release: In the uppermost layers of the epithelium, viral capsid proteins are synthesized, virions are assembled, and mature viruses are released as the epithelial cells naturally slough off.
Classification and Diversity
HPVs are classified based on the sequence of their L1 gene, with different types sharing less than 90% sequence identity. The current classification includes:
Genera: Five genera (Alpha-, Beta-, Gamma-, Mu-, and Nu-papillomaviruses) contain HPVs, with distinct tissue tropism and disease associations:
- Alpha-papillomaviruses: Primarily mucosal and genital types, including both high-risk and low-risk HPVs
- Beta-papillomaviruses: Primarily cutaneous types, often found in asymptomatic skin infections
- Gamma-papillomaviruses: Primarily cutaneous types, associated with various skin lesions
- Mu- and Nu-papillomaviruses: Less common cutaneous types
Types: Over 200 HPV types have been fully characterized, with many more partially characterized types identified through metagenomic studies.
Risk Classification:
- High-risk types (e.g., HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59): Associated with cervical and other anogenital cancers, as well as a subset of head and neck cancers
- Low-risk types (e.g., HPV 6, 11, 40, 42, 43, 44, 54, 61, 72): Associated with benign genital warts and low-grade cervical lesions
- Cutaneous types (e.g., HPV 1, 2, 4, 7): Associated with common skin warts
Role in Human Microbiome
Recent metagenomic studies have revealed that HPVs are much more prevalent in the human microbiome than previously recognized, with distinct HPV communities inhabiting different body sites:
Prevalence and Distribution
Overall Prevalence: Comprehensive metagenomic analyses of healthy individuals have shown an overall HPV prevalence of approximately 68.9%, with significant variation across body sites:
- Skin: 61.3% prevalence
- Vagina: 41.5% prevalence
- Mouth: 30% prevalence
- Gut: 17.3% prevalence
Type Diversity: The diversity of HPV types varies by body site, with many types showing strong organ tropism. Most HPVs detected in healthy individuals are not the high-risk types targeted by commercial HPV tests, suggesting a much more complex HPV community than previously appreciated.
Multiple Infections: Coexistence of multiple HPV types is common, occurring in approximately 48.1% of HPV-positive samples. Complex interactions between different HPV types, including both cooccurrence and exclusion patterns, have been observed, particularly in vaginal and skin samples.
Tissue Tropism
Different HPV genera and types show distinct tissue tropism:
Mucosal Sites:
- Alpha-papillomaviruses predominate in the genital tract and oral cavity
- Specific types show preferences for particular mucosal sites (e.g., certain types are more common in the cervix versus the vaginal fornix)
Cutaneous Sites:
- Beta- and gamma-papillomaviruses predominate on the skin
- Different body sites (e.g., face, hands, feet) harbor distinct HPV communities
Persistence: Many HPV infections in healthy individuals show remarkable persistence, with the same types detected in repeat samples collected months apart, suggesting true colonization rather than transient exposure.
Integration with Bacterial Microbiome
Emerging evidence suggests complex interactions between HPVs and the bacterial microbiome:
Vaginal Microbiome: The composition of the vaginal bacterial community appears to influence HPV infection and persistence:
- Lactobacillus-dominated microbiomes are associated with lower HPV prevalence and faster clearance
- Dysbiotic vaginal microbiomes with diverse anaerobes are associated with higher HPV prevalence and persistence
Oral Microbiome: Similar associations have been observed in the oral cavity, with certain bacterial communities potentially facilitating or inhibiting HPV infection.
Mechanistic Interactions: Proposed mechanisms for these interactions include:
- Bacterial modulation of the local immune environment
- Bacterial production of metabolites that influence HPV replication
- Alterations in epithelial barrier function
- Competition for receptor binding sites
Health Implications
The health implications of HPV infections range from completely asymptomatic to severely pathogenic, depending on the viral type, host factors, and site of infection:
Asymptomatic Infections
Prevalence: The majority of HPV infections in healthy individuals are asymptomatic and transient, with most immunocompetent hosts clearing the infection within 1-2 years.
Virome Component: Many HPV types appear to be commensal components of the human virome, particularly in the skin and mucous membranes, with no apparent pathogenic effects.
Immune Priming: Asymptomatic infections may play a role in priming the immune system, potentially influencing responses to subsequent HPV exposures.
Benign Proliferative Lesions
Cutaneous Warts:
- Common warts (verruca vulgaris): Caused primarily by HPV 2, 4, 7
- Plantar warts: Caused primarily by HPV 1, 2, 4
- Flat warts: Caused primarily by HPV 3, 10, 28
Anogenital Warts (Condyloma Acuminata):
- Caused primarily by low-risk types HPV 6 and 11
- Highly contagious but rarely progress to malignancy
- Can cause significant psychological distress and physical discomfort
Respiratory Papillomatosis:
- Caused primarily by HPV 6 and 11
- Characterized by recurrent growth of papillomas in the respiratory tract
- Can cause significant morbidity, particularly in the larynx where they may obstruct airways
Precancerous Lesions
Cervical Intraepithelial Neoplasia (CIN):
- Graded as CIN 1 (mild dysplasia), CIN 2 (moderate dysplasia), or CIN 3 (severe dysplasia/carcinoma in situ)
- Primarily associated with persistent infection by high-risk HPV types
- CIN 1 often resolves spontaneously, while CIN 2/3 has a higher risk of progression to invasive cancer
Vulvar, Vaginal, and Anal Intraepithelial Neoplasia:
- Similar grading system to CIN
- Associated with persistent high-risk HPV infection
- Risk factors include immunosuppression and cigarette smoking
Oral Potentially Malignant Disorders:
- Include leukoplakia and erythroplakia
- Subset associated with HPV infection, particularly in non-smokers
Malignant Neoplasms
Cervical Cancer:
- Nearly 100% attributable to high-risk HPV infection
- HPV 16 and 18 account for approximately 70% of cases worldwide
- Progression from persistent infection to invasive cancer typically occurs over 10-20 years
Other Anogenital Cancers:
- Vulvar cancer: Approximately 40% HPV-related
- Vaginal cancer: Approximately 70% HPV-related
- Anal cancer: Approximately 90% HPV-related
- Penile cancer: Approximately 50% HPV-related
Oropharyngeal Cancer:
- Increasing proportion attributable to HPV (particularly HPV 16)
- Distinct clinical and molecular profile compared to tobacco/alcohol-related cases
- Generally better prognosis than non-HPV-related cases
Non-melanoma Skin Cancer:
- Beta-HPV types may act as cofactors in the development of squamous cell carcinoma, particularly in immunosuppressed individuals and those with epidermodysplasia verruciformis
Host Factors Influencing Outcomes
Several host factors influence the clinical outcome of HPV infections:
Immune Status: Immunosuppression (due to HIV infection, organ transplantation, or other causes) increases the risk of persistent HPV infection, multiple HPV types, and progression to malignancy.
Genetic Factors: Host genetic polymorphisms in immune response genes and DNA repair pathways may influence susceptibility to HPV infection and progression.
Behavioral Factors: Smoking, long-term oral contraceptive use, and high parity increase the risk of progression from HPV infection to cervical cancer.
Microbiome Composition: As noted above, the local bacterial microbiome may influence HPV infection outcomes.
Metabolic Activities
The metabolic activities of HPVs are intimately linked to their replication strategy and interactions with host cells:
Viral Replication Strategy
Dependence on Host Machinery: HPVs have small genomes and encode few proteins, relying heavily on host cell machinery for replication:
- Utilize host DNA polymerases and replication factors
- Depend on host transcriptional machinery
- Exploit host cell metabolism for energy and building blocks
Cell Cycle Manipulation: HPVs manipulate the host cell cycle to create an environment conducive to viral replication:
- E7 protein (particularly from high-risk types) binds and inactivates pRb, forcing cells into S-phase
- E6 protein (particularly from high-risk types) targets p53 for degradation, preventing apoptosis
- These activities effectively uncouple cellular DNA synthesis from mitosis, allowing viral genome amplification
Metabolic Reprogramming
High-risk HPV infection induces significant metabolic reprogramming in host cells:
Glucose Metabolism: HPV-infected cells show increased glucose uptake and glycolysis, similar to the Warburg effect observed in cancer cells:
- Upregulation of glucose transporters (GLUT1)
- Increased expression of glycolytic enzymes
- Enhanced lactate production
Lipid Metabolism: HPV infection alters lipid metabolism to support viral replication:
- Increased fatty acid synthesis
- Upregulation of cholesterol biosynthesis
- Enhanced lipid droplet formation
Nucleotide Metabolism: HPV infection stimulates nucleotide biosynthesis to support viral genome replication:
- Upregulation of pentose phosphate pathway
- Increased expression of nucleotide biosynthetic enzymes
- Enhanced purine and pyrimidine synthesis
Redox Homeostasis: HPV infection modulates cellular redox status:
- Increased production of reactive oxygen species (ROS)
- Upregulation of antioxidant pathways to prevent excessive oxidative damage
- Exploitation of redox signaling for viral gene expression
Viral Protein Functions
The metabolic activities of specific HPV proteins include:
E6 Protein:
- Activates mTORC1 signaling, promoting protein synthesis and cell growth
- Enhances glucose uptake and glycolysis
- Prevents p53-mediated metabolic regulation
E7 Protein:
- Activates metabolic master regulators like c-Myc
- Enhances glutaminolysis
- Promotes nucleotide biosynthesis
E5 Protein:
- Enhances EGFR signaling, promoting glucose uptake
- Alters intracellular pH regulation
- Modifies membrane composition and trafficking
E4 Protein:
- Disrupts cytokeratin networks, potentially affecting cellular metabolism
- May influence cellular energy status in late stages of infection
Metabolic Interactions with Microbiome
Emerging evidence suggests metabolic interactions between HPVs and the local microbiome:
Vaginal Microbiome: Lactobacilli produce lactic acid, creating an acidic environment that may inhibit HPV infection and replication.
Oral Microbiome: Bacterial metabolites may influence HPV replication and persistence in the oral cavity.
Skin Microbiome: Interactions between cutaneous HPVs and the skin microbiome remain poorly understood but may involve metabolic crosstalk.
Clinical Relevance
The clinical relevance of HPVs encompasses their role in disease, approaches to detection and prevention, and therapeutic strategies:
Diagnostic Approaches
Cervical Screening:
- Cytology (Pap smear): Detects cellular abnormalities associated with HPV infection
- HPV DNA testing: Directly detects high-risk HPV types
- Co-testing (cytology plus HPV testing): Provides enhanced sensitivity
- Current guidelines increasingly favor primary HPV testing for cervical cancer screening
HPV Genotyping:
- Identifies specific HPV types present in a sample
- Useful for risk stratification and management decisions
- Particularly important for identifying HPV 16 and 18, which carry the highest risk
Biomarkers:
- p16/Ki-67 dual staining: Indicates HPV-induced cell cycle deregulation
- HPV E6/E7 mRNA detection: Indicates active viral oncogene expression
- Methylation markers: May identify lesions with higher risk of progression
Emerging Technologies:
- Next-generation sequencing: Allows comprehensive HPV typing and detection of variants
- Metagenomic approaches: Reveal the full spectrum of HPV types in the human virome
- Point-of-care tests: Enable rapid HPV detection in resource-limited settings
Preventive Strategies
Prophylactic Vaccination:
- HPV vaccines contain virus-like particles (VLPs) composed of the L1 protein
- Current vaccines include:
- Bivalent (HPV 16, 18)
- Quadrivalent (HPV 6, 11, 16, 18)
- Nonavalent (HPV 6, 11, 16, 18, 31, 33, 45, 52, 58)
- Highly effective at preventing infection and related diseases when administered before exposure
- Recommended for adolescents of all genders, with catch-up vaccination for young adults
Behavioral Interventions:
- Condom use provides partial protection against genital HPV transmission
- Limiting number of sexual partners reduces exposure risk
- Smoking cessation may reduce risk of progression from HPV infection to cancer
Screening Programs:
- Organized cervical screening programs have dramatically reduced cervical cancer incidence and mortality
- Integration of HPV vaccination and screening offers the potential for cervical cancer elimination
Therapeutic Approaches
Management of Benign Lesions:
- Cutaneous warts: Cryotherapy, salicylic acid, surgical removal
- Genital warts: Podophyllotoxin, imiquimod, cryotherapy, surgical removal
- Recurrent respiratory papillomatosis: Surgical debulking, adjuvant therapies
Management of Precancerous Lesions:
- Low-grade lesions: Often managed with observation due to high spontaneous regression rates
- High-grade lesions: Typically treated with excisional or ablative procedures
- Risk-based management incorporating HPV type and biomarkers is increasingly employed
Cancer Treatment:
- HPV status increasingly influences treatment decisions, particularly for oropharyngeal cancer
- De-escalation strategies for HPV-positive oropharyngeal cancer are under investigation
- Immunotherapies targeting HPV antigens show promise in early clinical trials
Therapeutic Vaccines:
- Unlike prophylactic vaccines, therapeutic vaccines aim to clear existing HPV infections
- Various approaches under investigation:
- Peptide/protein vaccines targeting E6/E7
- DNA vaccines
- Viral vector vaccines
- Cell-based vaccines
- Currently in clinical trials, with promising results for some approaches
Public Health Impact
Global Burden:
- Cervical cancer is the fourth most common cancer in women worldwide
- Over 600,000 new cases and 340,000 deaths annually
- Disproportionate burden in low- and middle-income countries
Economic Impact:
- Substantial healthcare costs associated with HPV-related diseases
- Productivity losses due to morbidity and premature mortality
- Cost-effectiveness analyses generally support HPV vaccination and screening
Health Disparities:
- Significant disparities in HPV-related disease burden and access to prevention
- Socioeconomic, racial/ethnic, and geographic disparities observed in many countries
- Addressing these disparities is a key public health priority
Interactions with Other Microorganisms
HPVs interact with other components of the human microbiome, including bacteria, fungi, and other viruses, with potential implications for infection outcomes:
Interactions with Bacteria
Vaginal Microbiome:
- Lactobacillus-dominated microbiomes are associated with lower HPV prevalence and faster clearance
- Bacterial vaginosis (characterized by diverse anaerobes) is associated with higher HPV prevalence and persistence
- Proposed mechanisms include:
- Production of lactic acid and bacteriocins by lactobacilli
- Modulation of local inflammation and immune responses
- Alterations in epithelial barrier function
- Production of metabolites that influence HPV replication
Oral Microbiome:
- Specific oral bacterial communities have been associated with HPV infection and persistence
- Periodontal disease may facilitate HPV infection through microabrasions and inflammation
- Certain oral bacteria may produce metabolites that influence HPV replication
Skin Microbiome:
- Interactions between cutaneous HPVs and the skin microbiome remain poorly understood
- Staphylococcus aureus colonization has been associated with certain HPV-related skin conditions
- Skin microbiome may influence local immune responses to HPV
Interactions with Other Viruses
HIV Coinfection:
- HIV infection increases risk of HPV acquisition, persistence, and progression to disease
- HPV infection may increase risk of HIV acquisition
- Mechanisms include:
- HIV-induced immunosuppression
- Shared routes of transmission
- HPV-induced inflammation and epithelial disruption
- Molecular interactions between viral proteins
Herpesvirus Coinfection:
- Herpes simplex virus (HSV) coinfection may facilitate HPV persistence
- Epstein-Barr virus (EBV) and HPV coinfection observed in some cancers
- Potential synergistic effects on cellular transformation
Hepatitis Virus Coinfection:
- Hepatitis B virus (HBV) and HPV coinfection may increase risk of cervical cancer
- Mechanisms may involve HBV X protein interactions with cellular pathways
Interactions with Fungi
Candida Coinfection:
- Candida albicans colonization has been associated with HPV persistence in some studies
- Mechanisms may involve:
- Candida-induced inflammation
- Alterations in local immune responses
- Changes in epithelial barrier function
Other Fungal Interactions:
- Limited research on interactions between HPV and other fungi
- Potential for indirect interactions through effects on local microenvironment
Polymicrobial Disease Concepts
Dysbiosis and HPV:
- Microbial dysbiosis may create an environment conducive to HPV infection and persistence
- HPV infection may, in turn, alter the local microbiome
- Bidirectional relationships create complex dynamics
Microbial Networks:
- Network analysis reveals complex interactions between HPV and other microorganisms
- Some interactions appear antagonistic, while others are synergistic
- These networks may influence disease outcomes
Therapeutic Implications:
- Modulation of the microbiome (e.g., probiotics) may influence HPV infection outcomes
- Combined approaches targeting both HPV and relevant microbiome components may be beneficial
- Personalized approaches based on individual microbiome profiles may be developed in the future
Research Significance
HPVs continue to be the subject of intensive research, with several key areas of current and future significance:
Virome Characterization
Metagenomic Approaches:
- Next-generation sequencing and metagenomic analyses are revealing the full diversity of HPVs in the human virome
- Many previously unrecognized HPV types are being discovered
- The functional significance of this diversity remains to be determined
Site-Specific HPV Communities:
- Different body sites harbor distinct HPV communities
- Understanding the factors that shape these communities is an active area of research
- Potential implications for site-specific disease risk
Temporal Dynamics:
- Longitudinal studies are investigating how HPV communities change over time
- Factors influencing acquisition, clearance, and persistence are being elucidated
- Developmental changes in the HPV virome from infancy to adulthood are being characterized
Microbiome Interactions
Mechanistic Studies:
- Molecular mechanisms underlying interactions between HPV and other microbiome components are being investigated
- In vitro and animal models are being developed to study these interactions
- Potential for identifying novel therapeutic targets
Clinical Implications:
- Microbiome profiles may serve as biomarkers for HPV infection risk and outcomes
- Microbiome modulation strategies may enhance HPV prevention and treatment
- Personalized approaches based on individual microbiome profiles are being explored
One Health Perspectives:
- Comparative studies of animal papillomaviruses and their microbiome interactions
- Evolutionary insights into papillomavirus-host-microbiome coevolution
- Potential zoonotic implications
Technological Advances
Single-Cell Approaches:
- Single-cell RNA sequencing is revealing heterogeneity in HPV gene expression within infected tissues
- Spatial transcriptomics is mapping HPV activity in the context of tissue architecture
- These approaches are providing new insights into HPV-host interactions
Organoid Models:
- Human epithelial organoids are enabling more physiologically relevant studies of HPV infection
- Co-culture systems incorporating immune cells and microbiome components are being developed
- These models facilitate mechanistic studies and therapeutic testing
CRISPR Technologies:
- CRISPR-based approaches are enabling precise manipulation of HPV genomes
- Host factors influencing HPV infection are being identified through CRISPR screens
- Potential therapeutic applications targeting HPV DNA are being explored
Therapeutic Innovation
Immunotherapeutic Approaches:
- Therapeutic vaccines targeting HPV antigens continue to be developed and refined
- Immune checkpoint inhibitors are being evaluated for HPV-associated cancers
- Adoptive T cell therapies targeting HPV antigens show promise in early studies
Antiviral Strategies:
- Small molecule inhibitors targeting HPV proteins or host factors required for HPV replication
- CRISPR/Cas-based approaches for targeted disruption of HPV DNA
- RNA interference strategies targeting HPV transcripts
Combination Approaches:
- Integration of conventional therapies with novel immunotherapeutic and antiviral approaches
- Microbiome modulation as an adjunct to HPV-targeted therapies
- Personalized approaches based on HPV type, host factors, and microbiome profiles
Global Health Perspectives
Cervical Cancer Elimination:
- WHO global strategy aims to eliminate cervical cancer as a public health problem
- Implementation research addressing barriers to vaccination and screening
- Novel approaches for resource-limited settings
Broader HPV Disease Burden:
- Increasing recognition of HPV's role in non-cervical cancers
- Evaluation of vaccination impact on these outcomes
- Economic analyses incorporating the full spectrum of HPV-related diseases
One Health Approaches:
- Comparative studies of papillomavirus ecology across species
- Insights from animal models of papillomavirus infection
- Potential zoonotic implications and evolutionary perspectives
In conclusion, Papillomaviridae represents a diverse and clinically significant family of viruses within the human virome. From their role as common commensal organisms in healthy individuals to their potential to cause malignant disease, HPVs exemplify the complex relationships between viruses and their human hosts. Ongoing research continues to reveal the full diversity of HPVs, their interactions with other microbiome components, and their impact on human health, with significant implications for disease prevention and treatment.
