Reduced Sleep-Disrupting Inflammation
Decrease the chronic inflammation that interferes with sleep quality through gut microbiome optimization for more restorative rest.
Key Supporting Microbes
These beneficial microorganisms play key roles in supporting this health benefit:
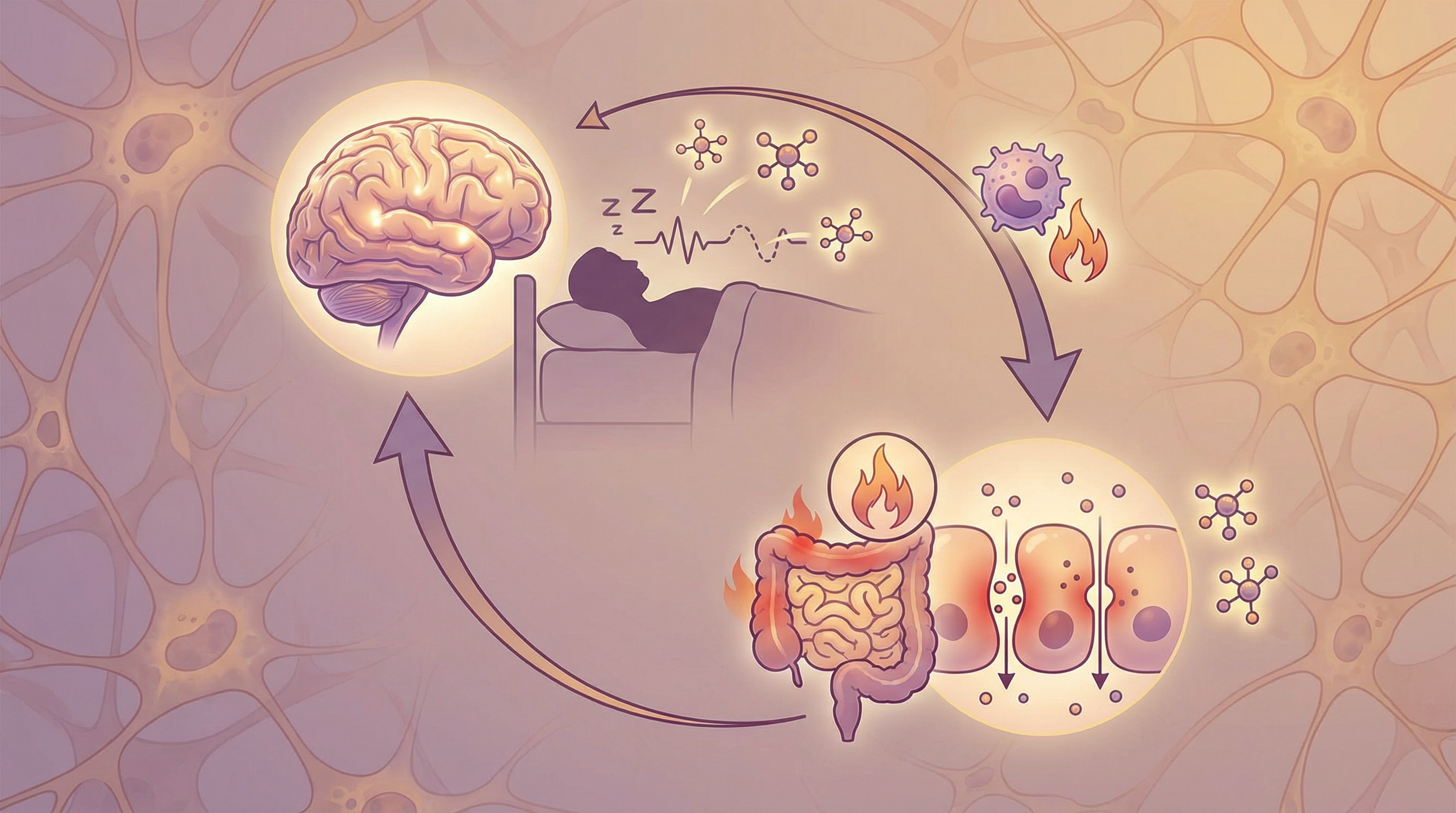
The Sleep-Inflammation Cycle
Sleep and inflammation have a complex, bidirectional relationship. Chronic inflammation disrupts sleep architecture, making it harder to fall asleep and reducing time in restorative deep sleep stages. Poor sleep, in turn, increases inflammatory markers—creating a vicious cycle that perpetuates both problems.[1]
Your gut microbiome sits at the center of this relationship, capable of either driving inflammation that disrupts sleep or producing anti-inflammatory compounds that support it.
How Inflammation Disrupts Sleep
Inflammatory Cytokines and Sleep
Specific inflammatory molecules affect sleep:[1]
IL-6 (Interleukin-6):
- Elevated in insomnia
- Causes fragmented sleep
- Increases time to fall asleep
- Reduces slow-wave (deep) sleep
TNF-α (Tumor Necrosis Factor-alpha):
- Associated with sleep disturbances
- Increases awakenings
- Reduces sleep efficiency
- Elevated in sleep apnea
IL-1β (Interleukin-1 beta):
- Affects sleep regulation
- In low levels, may promote sleep
- Elevated levels disrupt sleep
- Balance is key
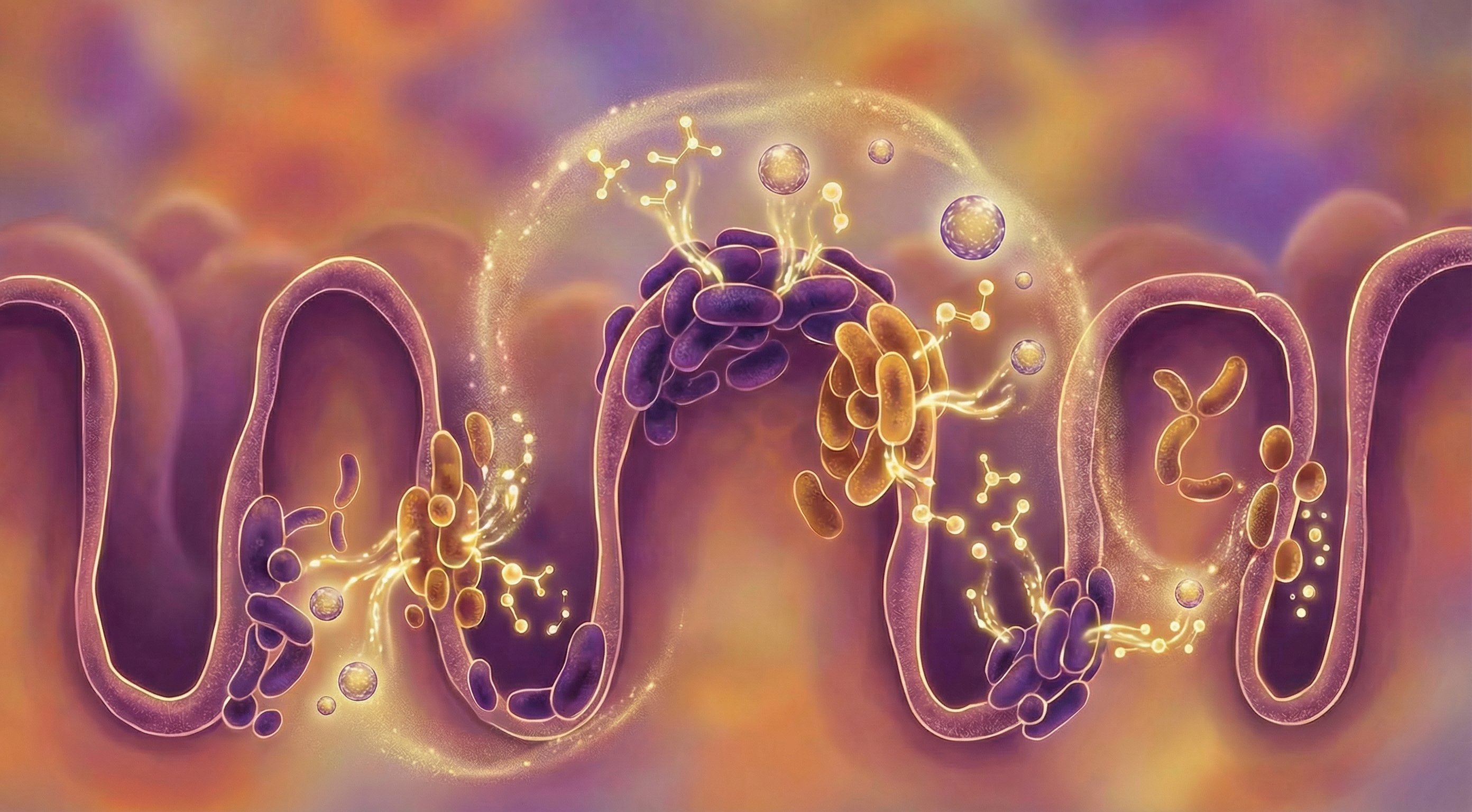
The Gut's Role in Sleep-Disrupting Inflammation
Gut dysbiosis drives inflammation that affects sleep:[2]
Leaky gut and LPS:
- Gut permeability allows bacterial products into bloodstream
- LPS triggers inflammatory cascade
- Creates systemic inflammation
- This inflammation reaches the brain and disrupts sleep
Inflammatory microbiome patterns:
- Certain bacteria promote inflammation
- Others have anti-inflammatory effects
- Balance determines inflammatory state
- Dysbiosis tips balance toward inflammation
Poor Sleep Worsens Gut Health
The reverse direction of the cycle:[3]
Sleep deprivation effects:
- Increases intestinal permeability
- Alters microbiome composition
- Increases inflammatory species
- Decreases beneficial bacteria
Creating the vicious cycle:
- Initial inflammation disrupts sleep
- Poor sleep increases gut permeability
- LPS leakage increases inflammation
- More inflammation, worse sleep
- Cycle perpetuates
Signs of Inflammation-Related Sleep Problems
Consider inflammation if you experience:
- Unrefreshing sleep despite adequate duration
- Difficulty achieving deep sleep
- Waking feeling achy or stiff
- Joint pain that's worse in the morning
- Brain fog on waking
- Frequent night awakenings
- Known inflammatory conditions
- Poor sleep alongside digestive issues
Key Anti-Inflammatory Microbes
Faecalibacterium prausnitzii
Most potent anti-inflammatory gut bacterium:
- Major butyrate producer
- Secretes anti-inflammatory proteins
- Often depleted in inflammatory conditions
- Supporting this species is key
Akkermansia muciniphila
Supports barrier and reduces inflammation:
- Maintains mucus layer integrity
- Reduces LPS translocation
- Associated with better metabolic health
- Responds to polyphenols
Bifidobacterium longum
Anti-inflammatory and sleep-supporting:
- Reduces inflammatory cytokines
- Some strains specifically help stress/sleep
- Produces anti-inflammatory metabolites
- Responds to prebiotic fibers
Roseburia Species
Important butyrate producers:
- Significant SCFA production
- Anti-inflammatory effects
- Support gut barrier
- Respond to dietary fiber
Dietary Strategies to Reduce Sleep-Disrupting Inflammation
Anti-Inflammatory Foods
Omega-3 fatty acids:
- Fatty fish (salmon, mackerel, sardines)
- Powerful anti-inflammatory effects
- Improve sleep quality in studies
- 2-3 servings weekly
Polyphenol-rich foods:
- Berries (especially tart cherries—also help sleep directly)
- Green tea
- Extra virgin olive oil
- Dark chocolate
- Colorful vegetables
Fiber for SCFA production:
- Diverse plant fibers
- Feed butyrate-producing bacteria
- Legumes particularly effective
- Reduce systemic inflammation
Pro-Inflammatory Foods to Avoid
Refined sugars:
- Spike inflammation
- Disrupt microbiome
- Worsen sleep
- Limit especially in evening
Processed foods:
- Contain inflammatory compounds
- Damage gut barrier
- Promote inflammatory bacteria
Excessive omega-6 fats:
- Industrial seed oils
- Shift balance toward inflammation
- Replace with olive oil
Alcohol:
- Increases inflammation
- Disrupts sleep architecture
- Damages gut barrier
- Avoid, especially near bedtime
Targeted Foods for Sleep and Inflammation
Tart cherry juice:
- Anti-inflammatory
- Natural melatonin source
- Shown to improve sleep
- 8oz tart cherry juice 1-2 hours before bed
Fatty fish:
- Omega-3s reduce inflammation
- Vitamin D supports sleep
- Studies show improved sleep quality
- Include several times weekly
Kiwi fruit:
- Anti-inflammatory compounds
- High antioxidants
- Studies show sleep benefits
- 1-2 kiwis before bed

Lifestyle Factors
Consistent Sleep Schedule
Regular sleep supports anti-inflammatory patterns:
- Irregular sleep increases inflammation
- Consistent timing reduces inflammatory markers
- Even on weekends
- Sets healthy circadian-immune rhythm
Stress Management
Chronic stress drives inflammation:
- Elevates inflammatory cytokines
- Disrupts gut barrier
- Worsens sleep
- Regular stress reduction essential
Exercise
Physical activity reduces inflammation:
- Regular moderate exercise is anti-inflammatory
- Improves sleep quality
- Supports healthy microbiome
- Time it right (not too close to bed)
Temperature
Cool sleeping environment:
- Supports natural body temperature drop
- May reduce inflammatory markers
- 65-68°F (18-20°C) typically ideal
- Use cooling bedding if needed
Breaking the Sleep-Inflammation Cycle
Interrupting the vicious cycle requires addressing both sides:
Improve gut health:
- Reduces inflammatory driver
- Supports anti-inflammatory bacteria
- Heals gut barrier
- Reduces LPS translocation
Improve sleep hygiene:
- Reduces inflammation from poor sleep
- Allows gut to repair overnight
- Supports healthy microbiome
- Creates positive cycle
Reduce inflammatory triggers:
- Diet modifications
- Stress management
- Environmental factors
Testing Inflammatory Status
If concerned about inflammation affecting sleep:
- hs-CRP: General inflammation marker
- ESR: Another inflammation indicator
- Inflammatory cytokines: IL-6, TNF-α (specialty testing)
- Microbiome testing: Can reveal inflammatory patterns
- Sleep study: If sleep disorders suspected
Building Better Sleep Through Reduced Inflammation
Reducing sleep-disrupting inflammation through the microbiome involves:
- Supporting anti-inflammatory bacteria with fiber and fermented foods
- Including omega-3s and polyphenols daily
- Eliminating pro-inflammatory foods especially in evening
- Healing gut permeability to reduce LPS translocation
- Maintaining consistent sleep schedule for circadian-immune health
- Managing stress which drives both inflammation and poor sleep
Most people notice improvements in sleep quality within 4-6 weeks of consistent anti-inflammatory dietary changes. Breaking an established sleep-inflammation cycle may take 2-3 months of sustained effort, but the improvements in both sleep and overall health are substantial.
Supporting Practices
Evidence-based strategies to support this benefit:
- Consume omega-3 fatty acids to reduce inflammation
- Include anti-inflammatory polyphenols from berries and green tea
- Eat high-fiber foods to produce anti-inflammatory SCFAs
- Limit refined sugars and processed foods
- Manage stress which promotes inflammation
- Maintain consistent sleep schedule to reduce inflammatory markers
References
- Irwin MR, Opp MR. Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity. Neuropsychopharmacology. 2017;42(1):129-155. doi:10.1038/npp.2016.148 ↩
- Poroyko VA, Carreras A, Khalyfa A, et al.. Chronic Sleep Disruption Alters Gut Microbiota, Induces Systemic and Adipose Tissue Inflammation and Insulin Resistance in Mice. Scientific Reports. 2016;6:35405. doi:10.1038/srep35405 ↩
- Reynolds AC, Paterson JL, Ferguson SA, et al.. The shift work and health research agenda: Considering changes in gut microbiota as a pathway linking shift work, sleep loss and circadian misalignment, and metabolic disease. Sleep Medicine Reviews. 2017;34:3-9. doi:10.1016/j.smrv.2016.06.009 ↩
