Neisseria gonorrhoeae
Neisseria gonorrhoeae, commonly known as gonococcus, is a gram-negative diplococcus bacterium that is an obligate human pathogen. It is the causative agent of gonorrhea, one of the most common sexually transmitted infections worldwide. Unlike some other members of the Neisseria genus, N. gonorrhoeae is exclusively pathogenic and not considered part of the normal human microbiome.
Key Characteristics
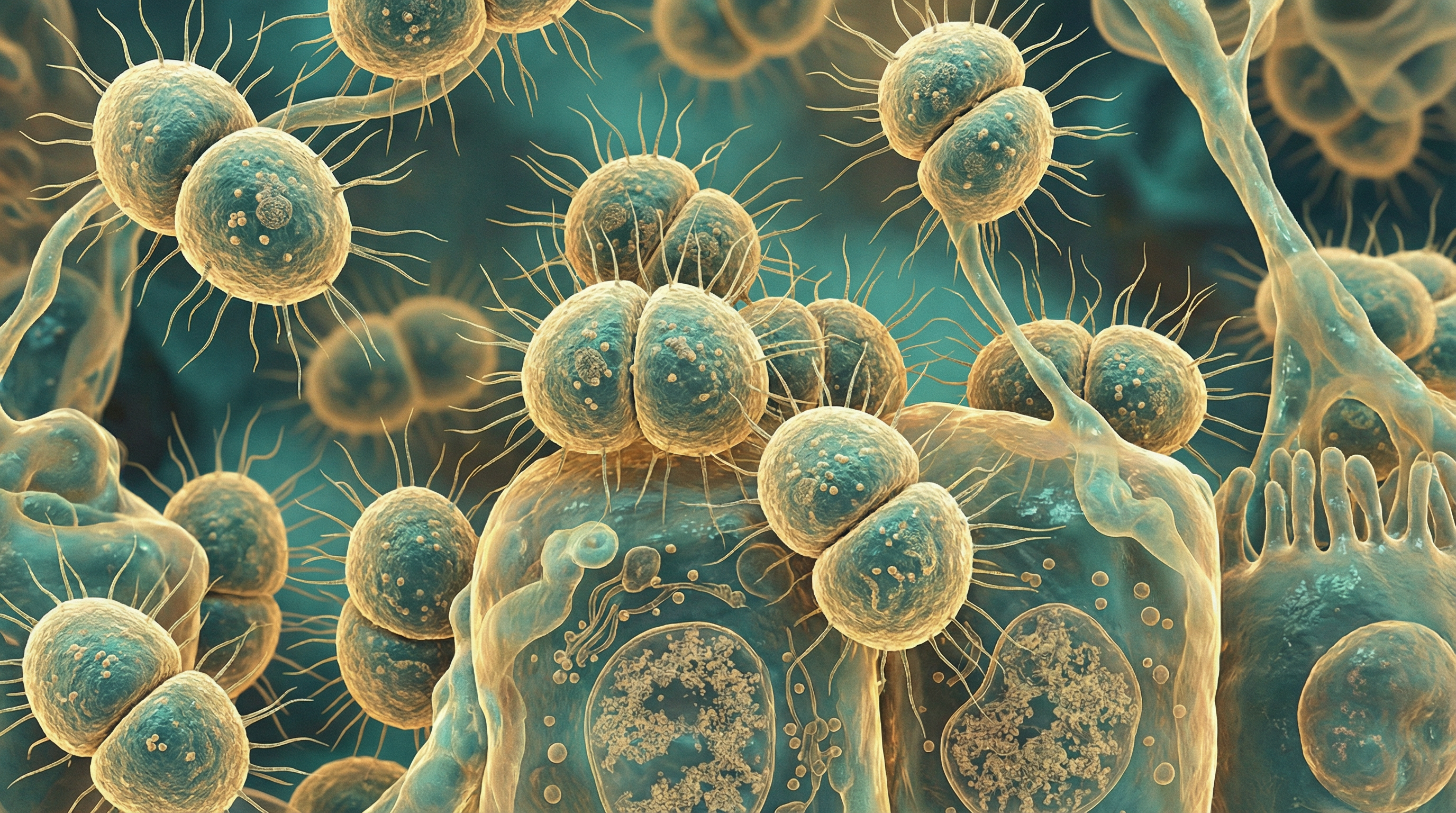
N. gonorrhoeae belongs to the family Neisseriaceae and appears microscopically as kidney bean-shaped cocci typically arranged in pairs (diplococci) with the concave sides facing each other. The bacterium is aerobic but can grow in microaerobic environments, is non-motile, and produces catalase and oxidase enzymes.
As a fastidious organism, N. gonorrhoeae requires complex media for growth, typically containing blood or serum supplements, and grows optimally at 35-37°C in a humidified environment with 3-7% carbon dioxide. It oxidizes glucose but not maltose or lactose, which helps distinguish it from other Neisseria species.
N. gonorrhoeae is a capnophile, requiring higher-than-normal concentrations of carbon dioxide for optimal growth. It lacks a polysaccharide capsule but possesses pili, opacity-associated proteins (Opa), and other surface structures that contribute to its virulence and ability to adhere to and invade host cells.
Role in Human Microbiome
N. gonorrhoeae is not considered part of the normal human microbiome. It is an obligate human pathogen that primarily colonizes and infects mucosal surfaces lined with columnar or pseudostratified epithelium, including:
- Urethral mucosa
- Endocervical mucosa
- Rectal mucosa
- Pharyngeal mucosa
- Conjunctival mucosa
The bacterium is transmitted through sexual contact or, in the case of neonatal infections, from mother to infant during childbirth. N. gonorrhoeae has evolved to be highly adapted to the human host, with no known animal or environmental reservoirs.
Health Implications
Pathogenic Potential
N. gonorrhoeae causes gonorrhea, a sexually transmitted infection that can manifest in various ways depending on the site of infection:
Urogenital gonorrhea:
- In males: Typically causes acute urethritis with purulent discharge and dysuria
- In females: May cause cervicitis, often with minimal symptoms, but can also present with vaginal discharge, dysuria, or abnormal menstrual bleeding
Extragenital gonorrhea:
- Pharyngeal infection: Usually asymptomatic but can cause sore throat
- Rectal infection: May be asymptomatic or cause proctitis with rectal pain, discharge, and bleeding
- Ocular infection: Causes conjunctivitis, particularly in neonates (ophthalmia neonatorum)
Disseminated gonococcal infection (DGI):
- Occurs in 0.5-3% of untreated infections
- Characterized by bacteremia, skin lesions, tenosynovitis, and septic arthritis
Complications
If left untreated, N. gonorrhoeae infection can lead to serious complications:
- In women: Pelvic inflammatory disease (PID), which can result in chronic pelvic pain, ectopic pregnancy, and infertility
- In men: Epididymitis, prostatitis, and rarely, infertility
- In both sexes: Increased risk of HIV acquisition and transmission
- Systemic complications: Endocarditis, meningitis (rare)
- In neonates: Blindness if ocular infection is untreated
Antimicrobial Resistance
N. gonorrhoeae has developed resistance to nearly all antibiotics used for treatment, making it an urgent public health threat. The World Health Organization has classified it as a "high priority" pathogen for research and development of new antibiotics. Current treatment typically involves dual therapy with ceftriaxone and azithromycin, though resistance to both drugs has been reported.
Metabolic Activities
N. gonorrhoeae has adapted to its human host with specialized metabolic capabilities:
- Utilization of glucose as a primary carbon source through oxidative metabolism
- Ability to use lactate, which is abundant in the genital tract, as an energy source
- Iron acquisition through specialized receptors for human transferrin, lactoferrin, and hemoglobin
- Production of IgA1 protease to cleave human immunoglobulin A
- Adaptation to microaerobic conditions found in mucosal surfaces
- Ability to survive oxidative stress through production of catalase and other antioxidant enzymes
These metabolic adaptations reflect its highly specialized niche as a human-restricted pathogen.
Clinical Relevance
The clinical significance of N. gonorrhoeae centers on its role as a major cause of sexually transmitted infections:
Epidemiology: The WHO estimates approximately 87 million new cases of gonorrhea occur annually worldwide, making it the second most prevalent bacterial STI after chlamydia.
Diagnosis: Includes nucleic acid amplification tests (NAATs), culture, Gram stain of urethral discharge (in symptomatic males), and point-of-care tests.
Treatment: Current recommendations include dual therapy with ceftriaxone plus azithromycin, though treatment guidelines evolve in response to antimicrobial resistance patterns.
Prevention: Condom use, regular screening of at-risk populations, partner notification and treatment, and potentially vaccine development (though no effective vaccine is currently available).
Antimicrobial resistance surveillance: Global programs monitor resistance patterns to guide treatment recommendations.
Interaction with Other Microorganisms
N. gonorrhoeae interacts with various members of the human microbiome:
Vaginal microbiome: Studies suggest that Lactobacillus-dominant vaginal microbiota may protect against symptomatic gonorrhea in women. Conversely, bacterial vaginosis-associated bacteria may enhance gonococcal survival.
Co-infections: Frequently co-occurs with Chlamydia trachomatis (in up to 50% of cases), which may influence the clinical presentation and treatment approach.
Horizontal gene transfer: N. gonorrhoeae can acquire DNA from other bacteria, including antibiotic resistance genes, contributing to its remarkable adaptability.
Biofilm formation: Can form biofilms in vitro and potentially in vivo, which may contribute to persistence and antibiotic tolerance.
Microbiome disruption: Gonococcal infection and subsequent antibiotic treatment can disrupt the normal microbiota at infection sites, potentially leading to secondary infections or dysbiosis.
Research Significance
N. gonorrhoeae remains an important focus of research for several reasons:
Antimicrobial resistance: As a "superbug" with resistance to multiple antibiotics, it serves as a model for studying the evolution and spread of resistance mechanisms.
Vaccine development: Despite decades of research, no effective vaccine exists, making it an important challenge in vaccinology.
Host-pathogen interactions: Understanding how N. gonorrhoeae evades the immune system and establishes infection provides insights into bacterial pathogenesis.
Point-of-care diagnostics: Development of rapid, accurate diagnostic tests is crucial for controlling spread, particularly in resource-limited settings.
Novel therapeutics: Research into new antibiotics, anti-virulence strategies, and immunotherapeutic approaches is ongoing.
Microbiome interactions: Studying how the local microbiome influences susceptibility to and outcomes of gonococcal infection may lead to new preventive strategies.
References
Unemo M, Shafer WM. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev. 2014;27(3):587-613.
Edwards JL, Apicella MA. The molecular mechanisms used by Neisseria gonorrhoeae to initiate infection differ between men and women. Clin Microbiol Rev. 2004;17(4):965-981.
Quillin SJ, Seifert HS. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat Rev Microbiol. 2018;16(4):226-240.
World Health Organization. Report on global sexually transmitted infection surveillance 2018. Geneva: World Health Organization; 2018.
Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548-562.
Lovett A, Duncan JA. Human Immune Responses and the Natural History of Neisseria gonorrhoeae Infection. Front Immunol. 2019;9:3187.
