The Gut-Skin Axis: How Your Microbiome Affects Skin Health, Acne, and Aging
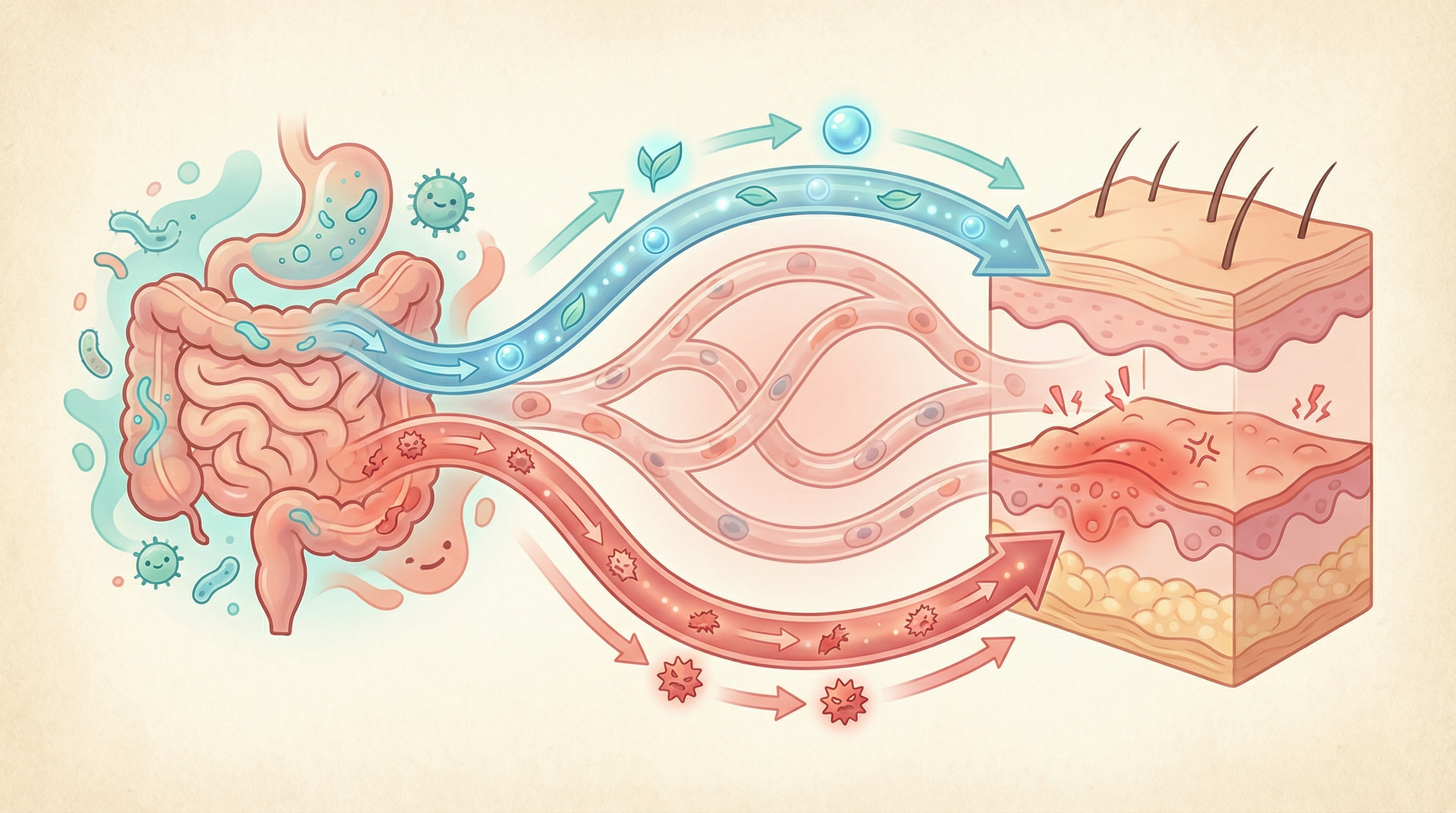
For decades, conventional dermatology focused almost exclusively on topical treatments and the skin's surface microbiome. However, emerging research reveals a powerful bidirectional connection between the gut and skin—what scientists now call the gut-skin axis[1]. Understanding this connection opens new possibilities for treating stubborn skin conditions from the inside out.
Understanding the Gut-Skin Connection
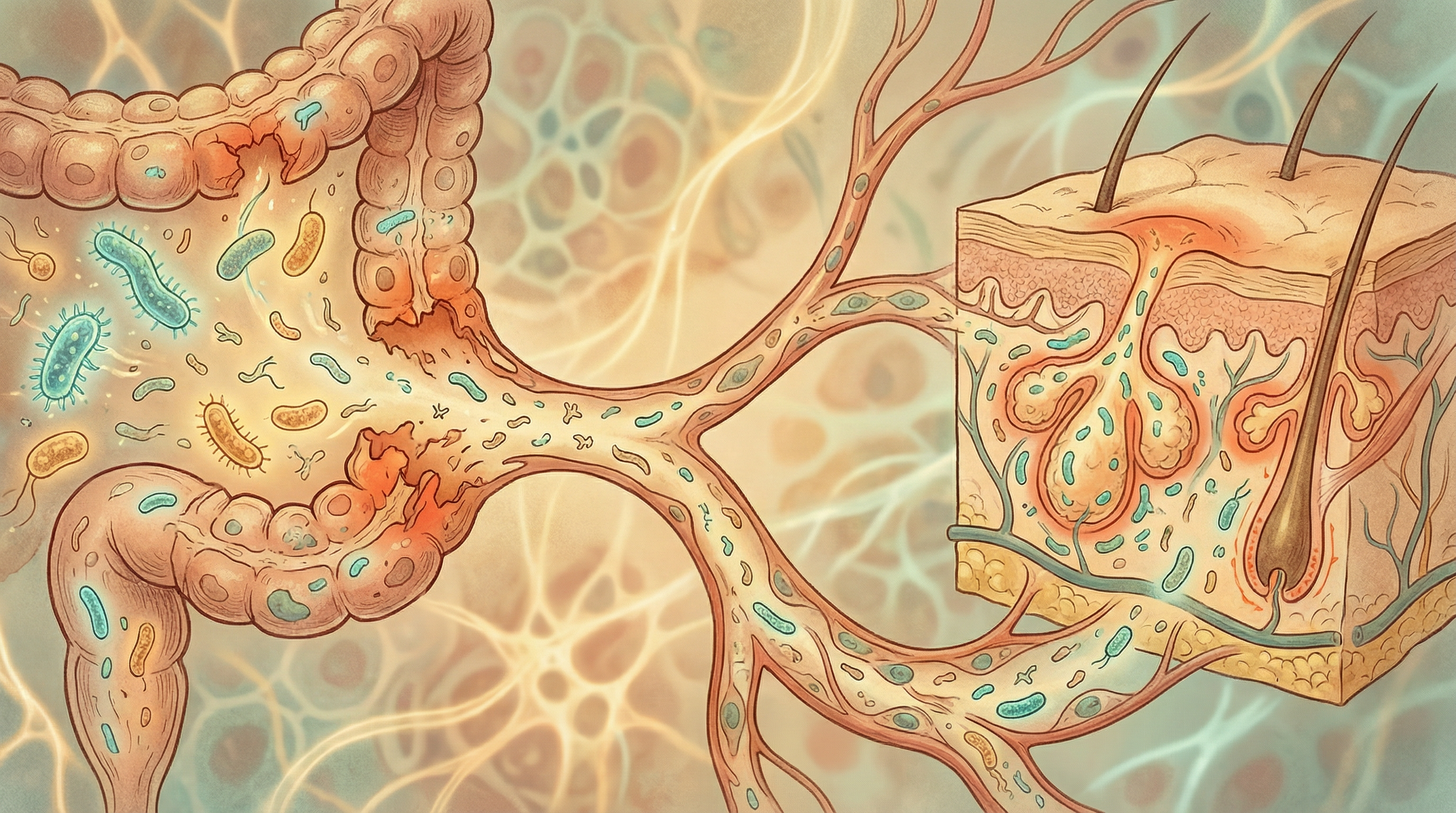
The gut and skin share several key features: both are densely populated with microorganisms, serve as barriers to the external environment, and play crucial roles in immune function. It's no surprise, then, that disruptions in gut health often manifest as skin problems[6].
How Gut Health Influences Skin
The gut-skin axis operates through several interconnected pathways:
Immune System Modulation Your gut microbiome trains and regulates the immune system. When gut dysbiosis causes immune dysregulation, the skin—as an immune-active organ—often displays the consequences through inflammation, sensitivity, and reactivity.
Systemic Inflammation Intestinal permeability ("leaky gut") allows bacterial products like lipopolysaccharides (LPS) to enter the bloodstream, triggering systemic inflammation that can manifest in the skin[1].
Metabolite Signaling Gut bacteria produce metabolites that travel through the bloodstream and influence skin cells. Short-chain fatty acids (SCFAs) from fiber fermentation have anti-inflammatory effects throughout the body, including the skin.
Nutrient Absorption Gut health affects absorption of skin-essential nutrients like zinc, vitamin A, essential fatty acids, and antioxidants. Malabsorption can lead to skin manifestations even when dietary intake is adequate.
Hormonal Regulation The gut microbiome influences hormone metabolism, including estrogen, testosterone, and insulin—all of which significantly impact skin health and conditions like acne.
Acne and the Gut Microbiome
Acne affects approximately 85% of people at some point in their lives. While traditionally attributed to hormones, genetics, and skin bacteria, research now highlights the gut's significant role[8].
Gut Dysbiosis in Acne Patients
Studies consistently find distinct gut microbiome patterns in people with acne[2]:
- Reduced overall microbial diversity
- Decreased beneficial Bifidobacterium and Lactobacillus
- Altered Firmicutes-to-Bacteroidetes ratios
- Lower SCFA production
The Gut-Brain-Skin Axis
Pioneering dermatologists Stokes and Pillsbury proposed the gut-brain-skin connection back in 1930. Modern research validates their theory[8]:
- Stress alters gut microbiome composition and intestinal permeability
- Gut dysbiosis promotes systemic inflammation
- Inflammation affects sebaceous gland function and skin barrier
- Skin symptoms (acne, oiliness, sensitivity) result
This explains why stress often triggers acne flares and why some people see skin improvements when addressing digestive issues.
Dietary Links
Foods that worsen both gut health and acne include:
- High-glycemic foods that spike insulin
- Dairy products (particularly skim milk)
- Excessive saturated fats
- Ultra-processed foods
Conversely, gut-friendly foods often improve acne:
- High-fiber vegetables and fruits (prebiotic-rich)
- Fermented foods with live cultures
- Omega-3 fatty acids from fish and flaxseeds
- Polyphenol-rich foods like berries and green tea
Eczema (Atopic Dermatitis) and Gut Health
Eczema is increasingly understood as a systemic condition with strong gut microbiome connections, particularly in its allergic (atopic) form[5].
The Early Life Connection
The gut microbiome's influence on eczema begins before birth:
- Maternal microbiome during pregnancy influences infant immune development
- Mode of delivery affects initial microbial colonization
- Infant feeding (breastfeeding vs. formula) shapes microbiome development
- Early antibiotic exposure correlates with increased eczema risk
Children who develop eczema often show reduced gut microbial diversity and lower levels of beneficial Bifidobacterium in infancy—sometimes months before skin symptoms appear.
Immune Dysregulation
Eczema involves inappropriate Th2 immune responses, leading to:
- Excessive IgE antibody production
- Mast cell activation
- Skin barrier dysfunction
- Chronic inflammation
A healthy gut microbiome promotes balanced immune responses and adequate regulatory T cells that prevent this type of overreaction[3].
Food Sensitivities
Many eczema patients have food sensitivities that worsen symptoms. Gut health influences this through:
- Intestinal permeability allowing food proteins to trigger immune responses
- Altered oral tolerance development
- Imbalanced immune regulation
Addressing gut health often reduces food reactivity and skin symptoms simultaneously.
Psoriasis: An Autoimmune-Gut Connection
Psoriasis is an autoimmune condition characterized by rapid skin cell turnover and chronic inflammation. Research increasingly implicates the gut microbiome in its development and severity[4].
Characteristic Gut Changes
Psoriasis patients consistently show:
- Reduced microbial diversity
- Decreased Akkermansia muciniphila (a key anti-inflammatory species)
- Lower Faecalibacterium prausnitzii (major butyrate producer)
- Altered Firmicutes-to-Bacteroidetes ratios
- Increased potentially inflammatory bacteria
Intestinal Permeability
Studies show increased intestinal permeability in psoriasis patients, allowing bacterial products to trigger systemic inflammation that perpetuates skin symptoms.
Comorbidities
The psoriasis-gut connection helps explain common comorbidities:
- Inflammatory bowel disease (IBD)—significantly more common in psoriasis patients
- Metabolic syndrome
- Cardiovascular disease
- Depression and anxiety
All these conditions share gut microbiome alterations as a potential unifying factor.
Skin Aging and the Microbiome
Beyond specific conditions, gut health influences skin aging and overall complexion:
Oxidative Stress
Gut dysbiosis increases systemic oxidative stress, accelerating skin aging through:
- Collagen breakdown
- DNA damage in skin cells
- Reduced antioxidant defenses
- Increased inflammation
Phenol Production
Certain gut bacteria produce phenolic compounds like p-cresol that accumulate in the skin and impair keratinocyte function. Studies show that improving gut health reduces skin phenol content and improves skin hydration and elasticity[7].
Nutrient Status
Gut health affects absorption of anti-aging nutrients:
- Collagen precursors (vitamin C, zinc, copper)
- Antioxidants (vitamins A, C, E, selenium)
- Essential fatty acids for skin barrier function
- B vitamins for cellular renewal
Strategies for Improving Skin Through Gut Health
Dietary Interventions
Increase prebiotic fiber:
- Inulin from garlic, onions, leeks, asparagus
- Resistant starch from cooled potatoes, green bananas
- Beta-glucan from oats, mushrooms
- Pectin from apples, citrus
Add fermented foods:
- Yogurt and kefir (choose unsweetened)
- Sauerkraut and kimchi
- Miso and tempeh
- Kombucha
Focus on anti-inflammatory foods:
- Fatty fish (salmon, sardines, mackerel)
- Colorful vegetables rich in polyphenols
- Extra virgin olive oil
- Turmeric and ginger
- Green tea
Reduce inflammatory triggers:
- Ultra-processed foods
- Refined sugars
- Excessive dairy (especially for acne-prone skin)
- Alcohol (disrupts gut barrier and dehydrates skin)
Targeted Supplementation
Probiotics for skin health: Research supports specific strains for skin conditions[1]:
- Lactobacillus rhamnosus GG – studied in atopic dermatitis
- Lactobacillus paracasei – may reduce skin sensitivity
- Bifidobacterium lactis – supports immune balance
- Lactobacillus plantarum – shows promise for acne
Prebiotics that support skin health:
- GOS (galactooligosaccharides) – promotes Bifidobacterium growth
- FOS (fructooligosaccharides) – supports beneficial flora
- Lactulose – prebiotic with additional benefits
Supportive nutrients:
- Omega-3 fatty acids for inflammation
- Zinc for wound healing and sebum regulation
- Vitamin D for immune modulation
- Collagen peptides for skin structure
Lifestyle Factors
Stress management: Stress directly impacts both gut and skin through the gut-brain-skin axis. Practices like meditation, yoga, adequate sleep, and regular exercise support both systems.
Adequate hydration: Water intake supports both gut function and skin hydration.
Quality sleep: Circadian rhythm disruption affects both microbiome composition and skin repair processes.
Minimize skin microbiome disruptors: While focusing on gut health, don't forget that harsh skincare products, over-washing, and environmental factors also influence the skin microbiome.

Testing and Personalization
Microbiome testing can provide insights into gut-skin connections:
What to look for:
- Overall microbial diversity
- Levels of anti-inflammatory species (Akkermansia, F. prausnitzii)
- Bifidobacterium and Lactobacillus abundance
- SCFA production capacity
- Potential dysbiosis markers
Correlating with skin symptoms: Track skin symptoms alongside gut health changes to identify personal triggers and effective interventions.
Working with Healthcare Providers
Optimal gut-skin management often requires collaboration between:
- Dermatologists for skin-specific treatment
- Gastroenterologists for digestive concerns
- Functional medicine practitioners for integrative approaches
- Registered dietitians for personalized nutrition
Be sure to share your full symptom picture, including both skin and digestive complaints, for comprehensive care.
The Future of Gut-Skin Medicine
Emerging research and treatments include:
- Topical probiotics containing beneficial bacteria for direct skin application
- Precision prebiotics tailored to individual microbiome profiles
- Postbiotics (bacterial metabolites) for systemic and topical use
- Fecal microbiota transplantation for severe inflammatory conditions
- Personalized nutrition based on microbiome analysis
Conclusion
The gut-skin axis represents a paradigm shift in understanding skin health. Rather than treating skin conditions purely from the outside, addressing the root causes through gut health optimization offers lasting improvements for many people.
Whether you're struggling with acne, eczema, psoriasis, or simply want healthier, more radiant skin, your gut microbiome deserves attention. The food you eat, the stress you manage, and the microbes you nurture all influence how your skin looks and feels.
Start your journey to better skin from within by exploring our skin health goals, learning about gut-supporting prebiotics, or considering microbiome testing to understand your personal gut-skin connection.
Your path to healthier skin might just begin in your gut.
References
- Salem I, Ramser A, Isham N, Ghannoum MA. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Frontiers in Microbiology. 2018;9:1459. doi:10.3389/fmicb.2018.01459
- Deng Y, Wang H, Zhou J, et al.. Patients with Acne Vulgaris Have a Distinct Gut Microbiota in Comparison with Healthy Controls. Acta Dermato-Venereologica. 2018;98(8):783-790. doi:10.2340/00015555-2968
- De Filippis F, Paparo L, Nocerino R, et al.. Specific gut microbiome signatures and the associated pro-inflammatory functions are linked to pediatric allergy and acquisition of immune tolerance. Nature Communications. 2021;12(1):5958. doi:10.1038/s41467-021-26266-z
- Huang L, Gao R, Yu N, et al.. Dysbiosis of gut microbiota was closely associated with psoriasis. Science China Life Sciences. 2019;62(6):807-815. doi:10.1007/s11427-018-9376-6
- Polkowska-Pruszyńska B, Gerkowicz A, Krasowska D. The gut microbiome alterations in allergic and inflammatory skin diseases – an update. Journal of the European Academy of Dermatology and Venereology. 2020;34(3):455-464. doi:10.1111/jdv.15951
- Sinha S, Lin G, Ferenczi K. The skin microbiome and the gut-skin axis. Clinics in Dermatology. 2021;39(5):829-839. doi:10.1016/j.clindermatol.2021.08.021
- Miyazaki K, Masuoka N, Kano M, Iizuka R. Bifidobacterium fermented milk and galacto-oligosaccharides lead to improved skin health by decreasing phenols production by gut microbiota. Beneficial Microbes. 2014;5(2):121-128. doi:10.3920/BM2012.0066
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future?. Gut Pathogens. 2011;3(1):1. doi:10.1186/1757-4749-3-1